The Complex Care Management program (CCM) at BMC is part of the MassHealth Accountable Care Organization (ACO) model in partnership with WellSense Health Plan. CCM serves patients across the Commonwealth and provides intensive care management services for patients presenting with three primary categories of complex needs:
- Behavioral health/substance use
- Chronic medical conditions
- Barriers related to social determinants of health
Our patients face significant personal and systemic barriers to accessing ambulatory care that meets their unique health needs, contributing to inequitable access to care and often higher inpatient and emergency department utilization and costs. These barriers are compounded by stigma related to race and ethnicity, mental health, substance use, socioeconomic status, and educational attainment/health literacy.
Our Mission
Our primary goal is to establish patients with ambulatory care and community-based supports to achieve patient-identified goals, improve health-related outcomes, and reduce avoidable hospital utilization
We aim to meet people where they are to improve access to care and health outcomes for those facing complex medical and psychosocial needs. Through collaboration, we coordinate care, address social barriers, and engage patients as active participants in their care. We strive to create a responsive healing environment with dignity and respect for the individuals and communities we serve.
Our Work
Patients enter the CCM program with minimal connection to primary care, specialty care, or community supports. They are often managing multiple chronic conditions, major behavioral health challenges, and health-related social needs. CCM partners with patients to improve their ability to manage their care and achieve their self-declared goals.
Staff work with patients through a combination of telephonic outreach and in-person encounters commonly in patient homes, clinics, shelters, hospitals, sub-acute nursing facilities, and other community-based settings. Staff coordinate care as needed with primary care and specialty providers via case conferences, in person interactions, messaging through the electronic health record, and/or phone; staff also work closely with home health agencies, inpatient care management staff, and community agencies. When patients are admitted to any type of inpatient facility, staff participate in planning transitions of care and outreach to the patient within 72 hours of discharge; they make every effort to visit patients in the home following discharge.
The team conducts weekly touchpoints with patients (or more frequent) early in the program, and the duration between touchpoints may lengthen as patients stabilize:
- RN/SW focuses on clinical coordination, navigation of clinical settings and resources, offers medication education and transitions of care support as well as connects to SUD resources
- CWA focuses on assessment of social determinants of health and navigation of social services, application assistance, transportation assistance and links to community resources
- Pharmacy performs medication reconciliation, medication education, streamlines refills and coordinates with prescribers
Through ongoing partnership with patients, CCM works to establish ambulatory care and community-based supports to achieve patient-identified goals, improve health related outcomes, and reduce avoidable hospital utilization.
Staff determine patients are ready for graduation when they have achieved the majority of their care plan goals, and have either demonstrated self-efficacy in sustaining health-related progress, or are connected to community-based and/or home health supports to sustain progress toward their goals. The median time to graduation is 15.2 months.
We use an intensive, face-to-face model based in a clinical setting, integrated with primary care and inpatient teams. Patients have multiple interactions per week across multiple settings and with multiple provider types — for example, a care manager may accompany patients to appointments.
Staffing Model
- Panel size: 45-75
- The core team is led by a registered nurse (RN) or social worker, along with a community wellness advocate and additional support from Pharmacy and our housing partners
- Transition of care intervention has a dedicated staff that provides individualized care while patients are in the hospital to address complex needs during hospital discharge.
CCM serves WellSense ACO patients with complex medical, behavioral health, and social needs.
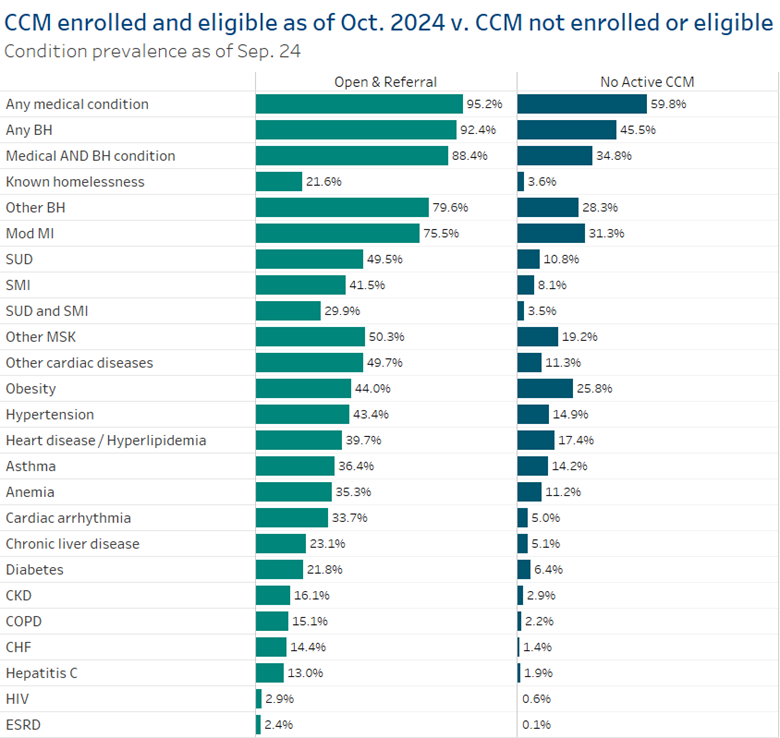
WellSense ACO (BACO, Mercy, Signature, Tufts, BILH) claims paid through September 2024
CCM enrollment and referral data through October 2024
Enrolled Boston Accountable Care Organization (BACO) members include:
- 40 percent Black
- 39 percent white
- Two percent Asian American and Pacific Islander
- 19 percent of undisclosed or unknown race.
In addition, 17 percent of BACO enrolled members are Hispanic/Latino, while 62 percent do not identify as Hispanic or Latino and 21 percent are of unknown ethnicity or have chosen not to disclose.
Risk
We find high and rising risk enrollees using two data-driven algorithms to select patients for impactibility and risk. Each list is updated every two months.
CAM Impactibility Score
This predictive risk algorithm is used to select top two percent highest risk adult patients. It incorporates:
- Demographics
- Utilization patterns
- Medication adherence and risk
- Diagnoses and clinical markers
- SDoH factors
- Risk scores (DxCG, Arcadia, HCC, etc)
PRISM Pediatric Risk Score
This predictive risk algorithm is used to select top two percent highest risk pediatric patients. It has a greater emphasis on engagement with specialty providers and diagnoses than on utilization, to account for the unique needs that pediatric patients have.
CCM teams are embedded in primary care, some specialty care, and inpatient settings across the WellSense network. We work with a variety of WellSense accountable care organizations across Massachusetts:
- Boston ACO (BACO): Greater Boston, Cape Cod, Fall River, Taunton
- BILH ACO: North Shore, South Shore, Greater Boston
- Care Alliance ACO: Lowell, Malden, Boston
- Mercy ACO: Springfield
- Signature ACO: Brockton, South Shore
Contact Us
If you're interested in how we got our start, email ccmoperations@bmc.org to learn more.
Referring to CCM
In addition to the algorithm, provider referrals and chart review confirms patients remain high-need and impactable. Provider referrals are a core identification source for CCM due to data lag and incomplete data that limits the sensitivity of predictive modeling. In addition, we are more successful engaging with referrals due to the established relationship,
Criteria for providers to consider includes:
- One inpatient stay OR three ED visits in six months
- Two chronic conditions
- SDoH barriers
- Identified opportunity for CCM impact
You can find the referral form on the WellSense website.
 en
en 
 Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español Tiếng Việt
Tiếng Việt Kreyol ayisyen
Kreyol ayisyen