- 2016: The Year in Review
- In Health Care, a Paradigm Shift Toward Addressing the “Why”
- What do you do, Sarah Kimball?
- Celebrating Our Commitment to Quality, Safety, and Patient Experience
- In Their Words
- News of Note
- Awards and Accolades
2016: The Year in Review

BMC had a busy year in 2016, from the celebration of the hospital’s 20th anniversary to major milestones in the clinical campus redesign to great work in the priority areas of quality, patient experience, and growth. Take a look back on what BMC accomplished this year.
January
- The new Women and Infants Center opened in the Yawkey Center. The new Center brings together the Ullian Neonatal Intensive Care Unit (NICU), Labor and Delivery, and all other hospital services for women from prenatal to postnatal care in a modern and comfortable setting for mothers and babies.
February
- BMC was awarded a $2 million grant from the National Institutes of Health's National Heart, Lung, and Blood Institute to study the impact of ambulance diversion on the outcomes of low-income patient populations across the United States. It is the first study of its kind to be funded by the NIH.
March
- An early warning system was launched on all adult medical-surgical floors at BMC. The system, which was highly praised by the Joint Commission, flags all adults non-critical care patients with clinical deterioration, so that doctors and nurses can intervene earlier and help reduce mortality.
April
- BMC helped 137 families file their taxes through StreetCred, a new program that helps patients fill out their tax returns and benefit from the full amount of refunds they are entitled to. In its first year, the program helped patients receive over $334,000 in returns, including $90,166 from the federal earned income credit. BMC was the first hospital in the country to offer a tax-assistance program for patients on site and will expand StreetCred to new clinics in 2017.
- BMC was named to Becker's Healthcare "150 Great Places to Work in Healthcare" for 2016. The annual list features provider organizations, including hospitals, health systems and ambulatory surgery centers, as well as nonprovider organizations, such as electronic health record providers and IT vendors. Winners are chosen based on workforce-centric awards received, benefits offerings, wellness initiatives, and efforts to improve professional development, diversity and inclusion, work-life balance, and a sense of community and unity among employees.
May
- The 20th annual BMC Gala, which was held on May 14, raised a record-breaking $4 million. The gala’s success came on the heels of Boston Medical Center crossing the threshold of $500 million in total funds raised since 1996. For the third year in a row, the Development Office is on track to surpass its $50 million annual goal to reach this milestone—a momentous and rare milestone for a safety-net hospital.
- BMC launched the Center for Transgender Medicine and Surgery, an innovative program that consolidates and coordinates the services BMC has previously been providing to transgender patients. With the opening of this center, BMC joined the small group of academic medical centers in the country providing comprehensive care to transgender individuals.
June
- The fourth annual Be Exceptional Awards honored 19 individual winners and six team winners. The winners were chosen for their exceptional performance and dedication to fulfilling BMC’s mission and the four QuEST goals: quality, efficiency, satisfaction, and total revenue.
- BMC’s Catwalk for Cancer raised more than $350,000 to help the Cancer Center fund transportation services for patients otherwise unable to get to appointments, complementary therapies such as yoga and acupuncture, and patient navigation services.
- The new cafeteria, The Teaching Kitchen, and Preventive Food Pantry opened in the Yawkey building, a major milestone in the clinical campus redesign. The comfortable new spaces provide staff and patients with an exceptional dining experience and allow for expanded classes in the Demo Kitchen and the ability to serve more patients in the food pantry.
- The BMC Board of Trustees named Barry Bock, RN; Pierre Cremieux, PhD; and Karen Kames as new BMC trustees, and Martha Samuelson Chair of the Board. James Phalen was named chair of the BMC Health System Board.
July
- July 1 marked the 20th anniversary of the joining of Boston City Hospital and Boston University Medical Center Hospital to form Boston Medical Center. Over those two decades, BMC has moved to the forefront of a new health care landscape, rising to meet the challenges of a changing health care environment, working together to achieve financial stability and expand our health system to provide more integrated, comprehensive care for patients and families, said Kate Walsh President and CEO.
- For the first time, BMC provided incoming interns with an orientation training module about social determinants of health, which are structural determinants and conditions that can affect health, such as socioeconomic status, employment, housing, and social support.
August
- Lisa Kelly-Croswell, Senior Vice President of Human Resources, was named a Woman of Influence by the Boston Business Journal.
- BMC expanded its physical and occupational services to a brand new location in Winthrop. This is the first offsite PT/OT location for BMC.
September
- BMC honored staff at different stages of their tenure, from five to 50 years, at the annual Service Awards. Kate Walsh, President and CEO, led the ceremony, which celebrated 668 staff members who have a collective 10,710 years of service. One staff person has been at BMC for 50 years and three have been at the hospital for 45 years.
- Boston Medical Center became the first hospital in Boston to launch an onsite baby café, continuing its commitment to providing ongoing care for new mothers in the local community.
- BMC HealthNet Plan’s MassHealth product was recently named one of the highest rated Medicaid health plans in the nation, receiving a rating of 4.5 out of 5 in the National Committee for Quality Assurance (NCQA) 2016-2017 Health Insurance Plan Ratings and a 4 out of 5 rating for its New Hampshire Medicaid product (Well Sense). This makes Well Sense the highest rated Medicaid health plan in New Hampshire.
October
- Researchers from Boston Medical Center and the Boston University School of Medicine, along with researchers from the University of California at San Francisco and the Vanderbilt University Medical Center, received $12.3 million in grant funding from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). This five-year grant will be used to further study the intersection between alcohol use and people living with HIV/AIDS.
- BMC was named one of the 50 greenest hospitals in America by Becker’s Hospital Review. Over the past few years, BMC has received the City of Boston Carbon Cup, increased our recycling rate by 50 percent in one year, and earned the Greenhealth Emerald Award for our sustainability efforts.
- Boston Medical Center formed an alliance with MIT and Post Office Square Redevelopment Corporation to buy electricity from a large new solar power installation, adding carbon-free energy to the grid. BMC was already on target to reduce its emissions by at least 50 percent by 2018 through a $300 million clinical campus redesign that includes upgrades to heating, cooling, and ventilation systems, a new biodigester to compost food waste, and other improvements.
November
- BMC revealed the results of a months-long journey to define how we collectively talk about our sense of pride and our focus for the future. This work led to a defined and articulated purpose – providing exceptional care without exception – and three values – built on respect powered by empathy, moving mountains, and many faces make our greatness. Coming together as an organization around BMC’s purpose and values will help the hospital reach its “audacious goal,” which is to make Boston the healthiest urban population in the world by 2030.
December
- Boston Magazine named 70 BMC physicians from 35 areas as "tops" in their respective fields.
In Health Care, a Paradigm Shift Toward Addressing the “Why”
This story is part of an ongoing series in the BMC Brief over the coming year on what the shift to a MassHealth ACO (accountable care organization) will mean for Boston Medical Center.
Health care is changing, and one major change under the Affordable Care Act is the emergence of accountable care organizations (ACOs), a delivery model designed to improve care coordination and reduce costs.
For Boston Medical Center and other providers, it will be a revolutionary change in MassHealth payment, from fee-for-service to a lump sum payment for each patient. The payment reform necessitates a different approach to patient care. To succeed under an ACO and reduce admissions, providers will need to identify the underlying cause of disease, and in many cases, find the right non-medical support for patients. It’s something that BMC is well prepared to do, having been a national leader on social determinants for decades, whether it was hunger, housing or other supports.
Thea James, MD, Vice President of Mission and Associate Chief Medical Officer, said the move to an ACO signals a long overdue change in the focus of the health care industry. For providers, a key responsibility will be asking “why?” – why a patient
may not be taking their medication, or coming to the Emergency Department repeatedly with the same chronic condition, or not following their doctor’s advice. The answers the patient gives could take the diagnosis in an entirely different direction.
“In the United States as a whole, we spend more money on health and have worse outcomes than in other countries,” says James, also an attending physician in the Emergency Department. “It’s clear that it doesn’t make sense for health care to go on this way, and so the health care system has had to look at what’s wrong with the current model. What’s been found is that there’s a lot of focus on the disease and not enough on why the disease is happening.”
Under an ACO model where hospitals are rewarded for keeping patients well, instead of just seeing patients for episodic care, the type of care that BMC already provides to patients will become even more important. From the Preventive Food Pantry to the Demonstration Kitchen to the Violence Intervention Advocacy Program, BMC is already focused on addressing social determinants of health – the structural determinants and conditions that can affect health, such as socioeconomic status, employment, housing, and social support.
“We are very lucky to be who we are and where we are right now,” says James. “We have always done what’s right, filling in gaps to enable our patients to benefit from care. We will continue to do what’s right, only now our approach will be slightly more nuanced, with a goal of making sure our patients have stable health and wellness along a continuum as well as removing any barriers to achieving this stability.”
According to James, there are many ways to begin to address social determinants of health.
“Engagement and asking questions are key,” says James. “It can be difficult to break yourself out of the cycle of assuming you know what your patient needs, but asking questions, expressing concerns, and generally showing compassion and empathy are key. Many people think that it takes more time to drill down to find the non-medical causes of disease, but what it really means is that we can get it right the first time and give our patients what’s most important and useful to them.”
Another key way to keep patients healthy is to leverage community-based services. These organizations will be key partners in interventions to address social determinants such as housing and helping BMC create sustainable models of care.
“Collaboration is essential,” says James. “We have a large footprint in the community, but we need to engage even more to make sure patients’ needs are met. This is also an area where listening to your patients can be key, as they can help you reach community services you might not even know exist.”
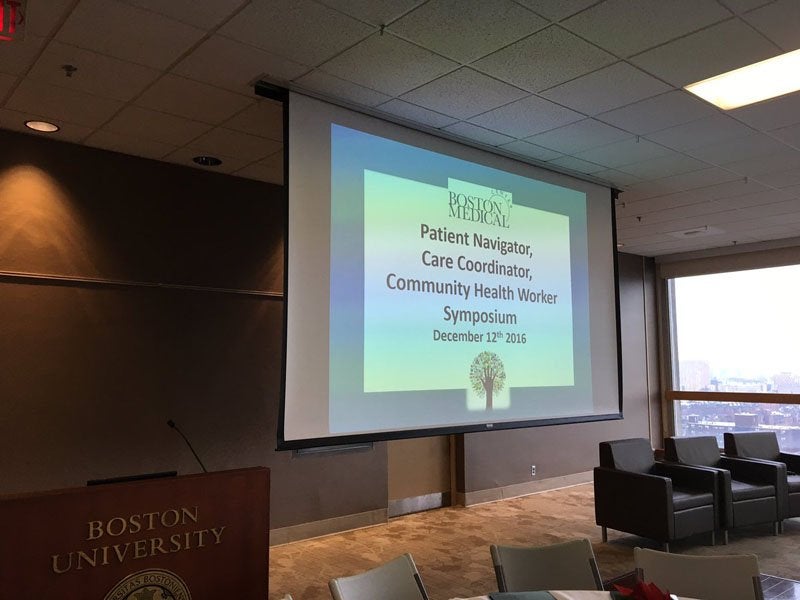
BMC’s reach into the community was on display on December 12, as BMC community health workers, care coordinators, and patient navigators gathered to discuss their work and the role of community health workers within the care system (pictured above). Under the ACO model, said Kate Walsh, president and CEO, community health workers will be critical in addressing disparities, understanding what keeps people trapped in the cycle of illness, and connecting patients to a spectrum of services that empower them.
A panel of community health workers discussed both the challenges and rewards of their roles. They noted that they’re able to touch people’s lives in their most vulnerable moments, and must build trust through talking with patients instead of judging them and displaying empathy and compassion. They also discussed the need for coordinated care, to ensure that patients get the help they need without feeling overwhelmed; care coordination is also a necessity under an ACO model.
James emphasized that once the intervention is in place, it’s equally important to follow the patient and document and measure the impact the intervention (e.g., housing) has had on both social and medical issues. This allows you to make adjustments when necessary, but also to measure return on investment and ensure that goals are being met.
“We need to integrate different streams of data to inform our intervention and tell us what we need to do to repair what is broken,” says James. “We provide this type of care because it’s the right thing to do, but now our payment models will align. We need to ensure that we’re spending money and resources in the right places in order to be successful.”
“BMC is very prepared for the upcoming health care shift to ACOs,” says James. “As an ACO, we will be given an opportunity to address social drivers of health instability with a new health care reimbursement model. We are quite fortunate to be who we are, as we have always been on this path. I’m so glad for the privilege to be here at this time and to have this amazing opportunity to partner with, collaborate with and support my colleagues on our campus and those in our communities to achieve such an exciting goal. We cannot throw away our shot.”
To read more about MassHealth and ACOs, read this story in the September 2016 BMC Brief.
What do you do, Sarah Kimball?
Name: Sarah Kimball, MD
Title: Primary care physician and director of resident education, Immigrant and Refugee Health Program
Time at BMC: Two years
Q: What do you do at BMC?
A: Half the time, I’m a clinical primary care physician, for both addiction and refugee clinical care. The other half of the time, I work on two projects – the Immigrant and Refugee Health Program and BeingWell, the internal complex care management program within General Internal Medicine.
For the Immigrant and Refugee Health Program, I do a lot of the administrative work to keep the refugee clinic running and to help facilitate getting potentially complex patients engaged in the US health care system. On Thursday afternoons, we have our main teaching clinic, where we do medical and psychological evaluations of refugees who have arrived in the United States less than 90 days before – we welcome them into the US health system. We do basic medical, public health, and mental health screenings, then get them engaged in primary care, either at BMC or somewhere close to where they live. We see about 250 new refugees in the clinic per year, plus 60 new consultations. For patients who decide to stay in our practice, I often become the long-term care primary care provider, along with our other attending physicians.
We also have a robust teaching program in the Immigrant and Refugee Health Program. This year, we have seven residents and three internal medicine fellows during each teaching cycle. We teach a combination of clinically relevant topics, such as tuberculosis and hepatitis B, and advocacy topics, such as how to use forensic skills rights to promote human rights.
Q: What brought you to BMC?
A: My husband works here, so I felt like I knew the BMC culture and mission. I always wanted to work in a place that actually lives the mission of caring for the underserved. In Boston, that place is very clearly BMC. I also wanted to be doing refugee health work and was an incredibly excited to learn an opportunity was available at BMC.
Q: What do you want people to know about the Immigrant and Refugee Health Program?
A: We’re available as a resource and take consults. We love to take care of these patients and are happy to work with anyone who has refugee or asylum seeking patients and needs extra support to take care of them. I think these patients are best taken care of by a multidisciplinary team, and I’m so grateful that we have such great collaborators. We have an integrated behavioral health team and we work closely with our colleagues at the Boston Center for Refugee Health and Human Rights, so we have the ability to provide wraparound services for patients whose trauma and past experiences may be influencing their ability to seek care. To send us consults, place an order in Epic for “Refugee Health in GIM.”
One way that other providers can determine if their foreign-born patients need more help is to ask them about how they got to the US and why they left their country of origin. We don’t often take the time to hear people’s migration histories, but within that story is their pre-migration story, their migration story, and their acculturation story. Understanding that trajectory helps me understand how vulnerable someone is, from both a health literacy and a trauma perspective. You can also find out from that story, someone’s current immigration status and how that affects their ability to access care.
People should also know that we can really help our patients by upholding the message that BMC is a safe place for people to come get their medical care and we will accompany them through whatever comes next.
Q: What do you like most about working at BMC?
A: I love working in a place where I can say that I want to do internal medicine from a human rights perspective and people know exactly what that means. The people I work with are people who love it here and love working in this environment.
But more than anything, it has to be the patients. They bring incredible diversity and richness. Even when the days are challenging, I’m here because I believe in the mission of what we do and why it’s important.
Q: Can you give me an example of a current case and how Immigrant and Refugee Health Program helped?
A: We’re currently seeing with a Somali refugee family, with a husband, wife, and seven children. The husband, who’s in a wheelchair from a gunshot injury to his spine many years ago in Somalia, actually came to the US before the rest of the family, the rest of whom arrived about nine months ago. We’ve been caring for the whole family as a team and helping them deal with issues such as housing instability, school readiness, and English literacy. We also did their green card paperwork through our Civil Surgeon program, and last week they came in and the dad announced to me that he was incredibly happy because we’ve made them an American family.
Moving along the pathway towards citizenship gives people many more rights and opportunities, so now they can get on public housing lists and apply for different services for their children, including one with cerebral palsy. One of the things I love about the Immigrant and Refugee Health program is that we are able to help patients not just with their medical care but also with some of the other socioeconomic supports that help them succeed, like citizenship.
Q: What do you do for fun outside of work?
A: I’m a Buddhist and have an active meditation practice. I’m also a big biker, and use that as my main mode of transportation and stress relief.
My husband and I have also been going to circus school to try to learn aerial silks. And I’m the mother of two cats.
Do you know a staff member who should be profiled? Send your suggestions to communications@bmc.org .
Celebrating Our Commitment to Quality, Safety, and Patient Experience
From November 14-18, the Boston Medical Center and Boston University School of Medicine communities came together to celebrate the fourth annual Quality, Safety, and Patient Experience Week, which featured department forums, a hospital-wide lecture, and a poster display.
On November 17, Keith Lewis, RPh, MD, chair of the Department of Anesthesiology at BMC and a professor of anesthesia at BUSM, presented “A Roadmap to Patient Safety” at the 12th Annual Raphael Miara Patient Safety Symposium. The Miara lecture is an ongoing commitment by Boston Medical Center to confront mistakes and learn from them, so something good can come of them.
Lewis began by using anesthesiology as an example of a discipline that has done much work to become safer, including technology advances, education, and adoption of practices from other high-risk industries. Anesthesiology had made these advances under the risk management safety hierarchy model, which Lewis said should be used as a model in other areas of medicine. This model includes eliminating as many risks as possible, implementing safety technologies and warnings/alarms, creating training guidelines, and using protective equipment.
When you’re about to do something potentially dangerous, said Lewis, there’s a simple method for proceeding – ensure that your level of preparedness and the level of complexity for whatever you’re about to do match. This helps ensure that you don’t waste resources by preparing too much or create a dangerous situation by preparing too little.
Lewis then discussed some of the safety work that has been undertaken at BMC, such as I-Cough, enhanced recovery after surgery, and trainings in the Alan D. Solomont Clinical Simulation and Nursing Education Center.
All of these factors, said Lewis, have made medicine at BMC safer, but the basics are still the most important part. “Respect and communication are key,” he said. “Close the loop, engage patients in the process, and lead by example when it comes to safety.”
Following the Miara Symposium, the audience moved to the Hiebert Lounge for the Quality, Safety, and Patient Experience poster ceremony and reception. Poster displays are an integral part of the week’s celebration, providing an opportunity for departments and teams to share their improvement strategies and celebrate their successes with the BMC and BUSM community. This year featured 37 posters, all of which highlighted the initiatives undertaken by BMC employees this past year to make the hospital safer for patients and provide them with a more positive experience. Awards were given for projects in five different categories: quality improvement, patient safety, quality research, innovative quality and patient safety curricula, and house staff. The poster teams were presented with their awards by Kate Walsh, president and CEO and Stan Hochberg, MD, senior vice president of quality, safety, and technology.
Award winners:
- Quality Improvement: Projects addressed quality improvement undertaken within the last year which demonstrated measurable improvements and sustainability over time.
- Leveraging the Electronic Medical Record to Reduce the Rate of Hospital Acquired Clostridium Difficile Infections
By Deborah Gregson; Nancy Miller, MD; Thomas Ostrander, MD; Bob Burke, RN, MA; Katherine Scanlon, RN, MSN; Matthew Bradley; Kelly Fleming; Youngjin Jung; Raagini Jawa, MD Pooja Jawa, MD; Muna Sheikh, MD; Jacob Walker; Cassandra Pierre, MD - Improving the Care of Vaso-Occlusive Episodes in the Adult Emergency Department
By Patricia L. Kavanagh, MD; Andrew Ulrich, MD; Carrie Solomon, MS; Evan Berg, MD; Elizabeth S. Klings, MD; Kelly Killius, PharmD; Lillian E. McMahon, MD; Mirinda Brown-Tyo, MSN, RN; Susan Griever, MS, RN; and Cristopher Amanti, MD - Initiation of a Pharmacologic Prophylaxis Program to Prevent Obstetric Associated Venous Thromboembolism
By Pooja Shah; Praachi Raje; Nick Thoreson; Jo Ann Thomas-Lewis; Rachel Shelley-Abrahamson; Ginny Combs, MSN, RNC-MNN, IBCLC; Lynne Lambert, RN; Susan Clark; Marie Kourtelidis, CNM; Julie Mottl-Santiago, CNM; Emma Trucks, MPH; Emily Jansen, MPH; Rhiannon Iorio, MPHc; Jodi Abbott, MD, MHCM; and Ron Iverson, MD - Reducing Length of Hospitalization for Neonatal Abstinence Syndrome Through Non-Pharmacologic Care & Methadones
By Elisha Wachman, MD; Susan Minear, MD; Bobbi Philipp, MD; Ginny Combs, MSN, RN; Karan Barry, RN; Kristine Smith, RN; Cathleen Dehn, RN, PhD; Donna Stickney, RN; Kate Mitchell; Rachel Goldstein; Nicole Penwill; Hira Shrestha, MA; Elizabeth Hutton, MD; Rachel Hoch, NP; Sheila Jane Lewis, NP; Rishitha Bollam; Nancy Desai; Jennifer Driscoll, RN, IBCLC; Robin Humphreys, RN, IBCLC; Hannah Simons, RN; Judy Burke, RN; Lauryl Ramakrishnan, NP; Camilla Farrell, PharmD; Katie Yasigian, SW; Jordana Price, MD6; Michelle Sia, DO; Kelley Saia, MD; and Davida Schiff, MD - Comprehensive Pharmacy Services Initiative to Improve Outcomes in Kidney Transplant Recipients
By Justine E. Dickson, PharmD; William R. Vincent III, PharmD; Jennifer Thurman, CPhT; Jean M. Francis, MD; and Matthew G. Nuhn, MD, FAC
- Leveraging the Electronic Medical Record to Reduce the Rate of Hospital Acquired Clostridium Difficile Infections
- Patient Safety: Projects with a focus on improving patient safety. The projects include those that may have been the result of a near miss, adverse event or from an identified risk.
- Novel Tool Utilized as a Trigger for Advance Care Planning in Hospitalized Oncology Patients
By Nicole Lincoln, MS, RN, APRN-BC, CCRN; Diane Sarnacki, MSN, RN, AOCN; Gretchen Gignac, MD; Alexandra Dobie, MSW, LCSW; Karla Damus, PhD, RN, MSPH, FAAN; and Sandhya Rao, MD
- Novel Tool Utilized as a Trigger for Advance Care Planning in Hospitalized Oncology Patients
- Quality Research: Research that demonstrates progress in quality improvement or patient safety. Projects include research development, testing and evaluation, and are designed to develop or contribute to generalizable knowledge.
- Opiate Over-prescription in Post-operative Patients
By Eric Y. Chen, MD,PhD and Paul Tornetta III, MD
- Opiate Over-prescription in Post-operative Patients
- Innovative Quality and Patient Safety Curricula: Projects that are educational in design and approach. Projects submitted should be tied to improving specific knowledge and skills tied to quality improvement and patient safety in trainees (students, residents, and fellows) and/or clinical and non-clinical staff.
- Maternal Code Blue Improvements after OB In Situ Simulations
By Shannon Bell, MD; Sheilah Bernard, MD; Andrew Camerato; Robert Canelli, MD; Pamela Corey, MS, RN; Elena Cotto; Janet Crimlisk, MS, RN; Ron Iverson, MD; Lynne Lambert, MS, RN; Ron Medzon, MD; Mark Norris, MD; Steven Poole; Frank Schembri, MD; Kristine Smith, RN, BSN
- Maternal Code Blue Improvements after OB In Situ Simulations
- House Staff Award: This award is in special recognition of a resident/fellow led effort, coming from any one of the five categories.
- Curricula: Improving Transitions of Care Through Implementation of IPASS Handoff Bundle - Multidisciplinary BMC Experience
By Aravind Ajakumar Menon, Emily M Jansen, Simy Kabaria Parikh, A Travis Manasco, Emma L Trucks, Mary Iaculli, Ryan Macht, Stephanie Le, Bhavna Seth, Maggie Collison, Juliet Fernandez, Aaron Richman, Jackson Steinkamp, Alex Iwamoto, Gazal Arora, Kalyn Reddy, Anshul Srivastava, Stephanie Talutis, Roxane Handal-Orefice, Melissa Markstrom, Sefira Bell-Masterson, James Moses, Rhiannon Iorio - Patient Safety: Interdisciplinary Communication Solutions from the Front-line
By Amma Agyemang, Temitope Awosogba; Joseph Benedict; Doreen Edmunds; Courtney Faiella; Laura Grenier; Karen Hogan; Stephanie Le; Sheila Murphy; Joanna Perdomo; Stephanie Talutis; John Tocio; Katherine Yee; Rena Zheng; Melissa Markstrom; and Nicole Lincoln
- Curricula: Improving Transitions of Care Through Implementation of IPASS Handoff Bundle - Multidisciplinary BMC Experience
This year, for the first time, the 2017 patient safety grant recipients were also announced at the poster reception. The recipients are:
- Prospective Review of Caprini Risk Assessment Model in Orthopaedic Surgery Patients
By Jesse Dashe, MD - Implementation of Best Practices to Reduce the Incidence of PICC Related Central Line Associated Blood Stream Infection (CLABSI)
By Cathy Korn, RN, MPH, CIC, Kellie Smith, RN, MSN, NE-BC, Cassandra Pierre, MD, MPH - Maximizing Safety and Efficiency with the Electronic Smart Nursing Assignment Program (SNAP)
By Kim Costello, MSN, RN,CMSRN, Molly Laferte, MSN, RN, OCN, Nicole Lincoln, MSN, RN, APRN-BC - Improving the Culture of Safety in Radiation Oncology via Implementation of Team STEPPS
By Yildirim D. Mutaf, PhD - Closed Loop Communication System for Completion of Recommended Follow-up on Radiology Studies
By Avneesh Gupta, MD - Improving MD/RN Interdisciplinary Communication to Address Patient Safety at BMC
By Nicole Lincoln, RN, Pamela Corey, RN - PASS – Priority Access for Severe Strokes
By Lauren Nentwich, MD, Sophia Dyer, MD, Hugo Aparicio, MD - Severe Hypertension in Pregnancy Bundle Initiation
By Ronald Iverson, MD
In Their Words
BMC frequently receives letters from patients sharing their experiences with the hospital. This letter was sent to Ravin Davidoff, MBBCh, SVP and Chief Medical Officer.
Hi Dr. Davidoff,
I wanted to touch base with you to let you know what a positive experience I had at Boston Medical Center. On November 16, I had the VT ablation procedure performed by Dr. Helm and his team. From the moment I entered the hospital, until I was discharged later in the day, everyone I encountered was professional, explaining everything that was happening and ensuring both myself and my family were comfortable throughout. Along with Dr. Helm, the nurse I had that day, Mark, couldn't have been more helpful and the nurse practitioner who also followed me that day and who I saw a week after the procedure was also wonderful, all spending the time to ensure my questions were answered and that I was feeling well. I truly can't say enough good things about the care I received.
With sincere thanks.
Quincy, MA
News of Note
Tracy Battaglia, MD, Named Board Chair of American Cancer Society New England Division
Tracy Battaglia, MD, a primary care physician at BMC, associate professor of medicine and epidemiology at BUSM, and director of the Center of Excellence in Women’s Health, has been appointed as the board chair of the American Cancer Society’s New England Division for a one-year term. Battaglia has volunteered with the American Cancer Society for over two decades and has held numerous positions on the New England Division Board of Directors.
Awards and Accolades
BMC Doctors Named “Top Docs” by Boston Magazine
Seventy BMC doctors were included on the annual Boston Magazine list of “Top Docs.” As in years past, BMC was strongly represented in numerous fields and specialties. In addition, BMC’s Long Life Family Study was also highlighted in the Top Docs issue, showcasing BMC’s commitment to research that will help improve the health of future generations.
BMC Honored with a Food Recovery Challenge Regional Award
BMC has received a Food Recovery Challenge Regional Award from the federal Environmental Protection Agency. The award recognizes BMC’s outstanding accomplishments in preventing and diverting wasted food.
BMC Researcher Receives Award for HIV Work in Russia
The Prix Galien Russia Committee, which honors the achievements of the best research team in the pharmaceutical field working in Russia, awarded a Special Jury Award to a team of researchers that includes Jeffrey Samet, MD, MA, MPH, chief of the Section of General Internal Medicine. The award honors the team’s research on the prevalence of HIV in vulnerable populations in the Russian Federation.
