BMC conducts high quality research that broadens and deepens our understanding of addiction treatment and care delivery so that successful approaches can be extended to more patients in need. The Grayken Center for Addiction at Boston Medical Center is increasing the pace of innovative research and evaluating new models of care delivery to create pathways to long-term recovery throughout the health care system.
Selected Current Research Projects
 Embracing Anti-Racism in Addiction Treatment, Research, and Policy Convening
Embracing Anti-Racism in Addiction Treatment, Research, and Policy Convening
The Substance Use and Anti-racism (SUDA) Research Program launched at the end of spring 2021. It is a community-engaged process to improve addiction treatment for Black patients. The guiding question is, “How can we make addiction treatment more appealing, effective, and equitable for Black patients?”
In the earliest phase of the project, researchers integrated a range of methods, including focus groups with Black patients who have substance-related problems and live in the neighborhoods surrounding BMC, and six scoping literature reviews to understand key factors that shape Black people’s experiences of addiction treatment. This later led to the next phase funded by the Patient Centered Outcomes Research Institute.
To learn more about this research, click here.
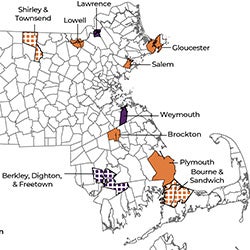
HEALing Communities Study
BMC has the distinction of being the recipient of the largest grant awarded by the US government to combat the opioid epidemic. Scientists from the nation’s leading health agencies and four major academic institutions are partnering with communities in four states to test a set of interventions to combat the opioid crisis. The ambitious HEALing Communities Study aims to reduce opioid overdose deaths by 40 percent over 3 years in participating communities. The Massachusetts team is led by Grayken faculty member Dr. Jeffrey Samet, Chief of BMC’s Section of General Internal Medicine. The study website shows the communities that are partnering with BMC to implement measures that are aimed at drastically cutting deaths from opioid overdose in the next few years.
Learn more about the HEALing Communities Study
For more information, contact Carly Bridden, MA, MPH, HEALing Communities Study, Carly.Bridden@bmc.org

Improving Physician Opioid Prescribing for Chronic Pain in HIV-infected Persons
The "Targeting Effective Analgesia in Clinics for HIV" (TEACH) Study RCT tests whether a collaborative care intervention for physicians improves the delivery of chronic opioid therapy for HIV-infected persons.
Substance Use Professionals' Experiences During COVID-19: A Focus on Outpatient Therapy
This qualitative research study focuses on how the COVID-19 pandemic has influenced substance use professionals’ experiences in providing outpatient therapy for opioid use disorder in Massachusetts. Eligible participants will have worked for two or more years in outpatient therapy for opioid use disorder, with at least one of those years during the COVID-19 pandemic. Broadly, the purpose of this research study is to explore the intersection between the Massachusetts’ opioid epidemic and the COVID-19 pandemic through the perspective of substance use professionals, as well as provide a means to gather insights into outpatient therapy modalities adopted during the pandemic.
Interested professionals may contact Caitlyn Leonard at caitlynl@bu.edu or (978) 826-3959. Compensation is available

Research in Addiction Medicine Scholars (RAMS)
The NIDA-funded Research in Addiction Medicine Scholars (RAMS) Program will develop skills in addiction medicine research among physicians from ABAM Foundation-accredited addiction medicine fellowship programs or addiction psychiatry fellowship programs across the United States. The RAMS Program will make important contributions to the development of the next generation of addiction physician researchers in order to provide better care for patients with and at risk for addictive diseases.

RESPECT Perinatal Substance Use Research Group
More than 120 babies are born at BMC each year to women with opioid use disorders. Researchers in the Departments of Pediatrics & Obstetrics and Gynecology are busy discovering new and better treatments for these vulnerable infants, many of whom are develop Neonatal Abstinence Syndrome (NAS). All babies born to with in-utero opioid exposure are monitored as inpatients for 5-7 days for symptoms of opioid withdrawal. The most recent available data suggest that twelve percent of all NAS babies in the state are cared for by BMC.
The RESPECT Research Group is learning about the short-term medical and long-term developmental outcomes of treating these newborns with different pharmacologic regimens. The groundbreaking studies conducted by the RESPECT Research Group are resulting in many publications, leading the way to higher quality, more personalized care for babies exposed to opioids during pregnancy.
Recent studies and publications have focused on the impact of buprenorphine or naltrexone treatment on NAS outcomes, the impact of genetic variants on NAS outcomes, the influence of clinical factors such as prematurity and breastfeeding on NAS outcomes, and the importance of non-pharmacologic care on NAS outcomes.

Targeting HIV-comorbidities with Pharmacotherapy to Reduce Alcohol and Tobacco Use in HIV-infected Russians
The St PETER HIV trial will to compare the effects of two nicotinic receptor partial agonists, varenicline and cytisine, on alcohol consumption, alcohol craving, smoking, inflammation, CHD risk and mortality risk.

TOPCARE
There is evidence to suggest that many individuals suffering from opioid use disorders become addicted after having been legally prescribed opioids by a physician as a treatment for chronic pain. In all-too-many cases, prescription opioid use escalates to a heroin addiction, as heroin is cheaper and easier to access than prescription opioids.
The purpose of TOPCARE (Transforming Opioid Prescribing in Primary Care) is to bring change in the way primary care services are delivered and decrease misuse of, and addiction to, prescription opioids.
With federal research funding, BMC physician researchers are examining the impact of opioid prescribing guidelines for chronic pain to determine whether adherence to these guidelines reduces opioid misuse. The TOPCARE program trains physicians to adhere to prescribing guidelines and then follows up with physicians implementing the guidelines to continue to improve prescribing of targeted drugs.
TOPCARE is expected to improve patient care, prevent addiction, and reduce healthcare costs.
Racism, Not Race: a Quantitative Analysis of the Use of “Race” and “Racism” in the Addiction Literature
Racism plays a unique role in the way that substance use and addiction are conceptualized and treated in the United States. Yet it is known from a prior study that medical journals are unlikely to name “racism” even when the same article mentions “race.” We sought to repeat this analysis among addiction medicine journals, hypothesizing that articles in addiction medicine journals would be more likely to discuss both race and racism. Analyzing articles in the past 30 years in five prominent addiction medicine journals, we found that race was mentioned not uncommonly, but that racism was mentioned vanishingly rarely, in less than 1% of articles. In our paper, we argue that this enforced ignorance on the topic of racism in addiction contributes to racialized policies and treatment systems.
Inequities in buprenorphine initiation, engagement, retention among patients at Boston Medical Center
Opioid overdose deaths continue to accelerate with a disproportionate rise among individuals from historically marginalized groups, especially individuals who are Black, Latino or Indigenous. In addition, these groups exhibit lower receipt of buprenorphine, a key medication in the treatment of opioid use disorder (OUD), relative to White individuals. Similar patterns emerge at the neighborhood-level. For example, research has identified associations between neighborhood-level race, ethnicity and income with rates of treatment with buprenorphine and other medications for OUD (MOUD). This proposal leverages the Data 4 Equity (D4E) platform, an effort by the BU CTSI Biomedical Informatics Core to strengthen geo-spatial and health disparities research at BUMC. The proposed research aims to describe individual and neighborhood-level disparities in buprenorphine receipt for BMC patients using D4E. This proposal will generate the preliminary work needed for a larger proposal involving more robust geo-spatial analyses of disparities in buprenorphine treatment at BMC.
Harm Reduction Policies and Practice in Massachusetts Homeless Shelters
Overdose remains the leading cause of death among people experiencing homelessness. Harm reduction practices can improve engagement with people who use drugs and decrease chance of fatal overdose, but attitudes and policies regarding substance use can vary widely between shelters. We seek to describe the range of harm reduction policies in place in shelters in Massachusetts by interviewing shelter staff and guests in 4 shelters in 4 communities across the state. We also plan to develop a set of practical harm reduction best practices as well as promising future practices for shelter-based harm reduction based on interviews with staff and guests.
HEAL Initiative: Preventing Opioid Use Disorder in Older Adolescents and Young Adults Disorders
The HEAL Prevention Cooperative is a multi-site NIH Initiative aiming to make evidence-based preventive intervention services available and accessible to all persons who experience risk for opioid and other substance misuse or disorder. At BMC, in conjunction with MGH, the team is conducting a naturalistic longitudinal observational study assessing the impact of treatment of psychopathology (mental health disorders) on the development of OUD, SUD, and nicotine use disorders in young people (16 to 30 years) who engage in behavioral health treatments.
The SAFEST Choice Learning Collaborative
The SAFEST (SBIRT and FASD Education, Support, and Technical assistance) Choice Learning Collaborative is a national educational program that aims to reduce the incidence of prenatal alcohol exposure (PAE) and improve outcomes in children with suspected or diagnosed fetal alcohol spectrum disorders (FASD). SAFEST Choice uses a Project ECHO virtual education model to train interdisciplinary pediatric and prenatal health care teams on how to screen for and counsel patients about the risks of alcohol use during pregnancy, and how to identify and care for children and adolescents with suspected or diagnosed FASD.
Impact of initial buprenorphine prescribing strategies on retention in care for patients with opioid use disorder
Treatment of opioid use disorder with the medication buprenorphine reduces risk of opioid overdose mortality, but poor retention in care limits this medication’s protective effect. This proposal will use large observational data to examine the relationship between buprenorphine dosage strategies and retention by: 1) describing current buprenorphine dosage practices in terms of dosage trajectories, 2) comparing the effect of two distinct buprenorphine dosage strategies on retention, and 3) estimating the impact of improved buprenorphine dosage practices on retention and overdose for the state of Massachusetts. This proposal has the potential to identify improved buprenorphine dosage strategies that increase retention in care, a key pillar in reversing the opioid overdose epidemic. .
Recent Publications by Grayken Faculty
Johnson, N.L., Beaugard, C.A., Heredia-Perez, D., So-Armah, K. Reason, P., Yule, A.M., Lee, C.S., Chapman, S.E., Chatterjee, A., McClay, C., Weeden, T., Becerril, C., Thomas, D., Komaromy, M. (2024). Embracing anti-racism: Co-creating recommendations with Black people for how addiction treatment needs to change,
Social Science & Medicine, 364. https://doi.org/10.1016/j.socscimed.2024.117433.
Basukala, B., Rossi, S., Bendiks, S., Gnatienko, N., Patts, G., Krupitsky, E., Lioznov, D., So-Armah, K., Sagar, M., Cheng, C., & Henderson, A. J. (2023). Virally Suppressed People Living with HIV Who Use Opioids Have Diminished Latency Reversal. Viruses, 15(2), 415. https://doi.org/10.3390/v15020415
Mustanski, B., Saber, R., Jones, J. P., Macapagal, K., Benbow, N., Li, D. H., Brown, C. H., Janulis, P., Smith, J. D., Marsh, E., Schackman, B. R., Linas, B. P., Madkins, K., Swann, G., Dean, A., Bettin, E., & Savinkina, A. (2023). Keep it up! 3.0: Study protocol for a type III hybrid implementation-effectiveness cluster-randomized trial. Contemporary clinical trials, 107134. Advance online publication. https://doi.org/10.1016/j.cct.2023.107134
Bertholet, N., Winter, M. R., Heeren, T., Walley, A. Y., & Saitz, R. (2023). Polysubstance Use Patterns Associated With HIV Disease Severity Among Those With Substance Use Disorders: A Latent Class Analysis. Journal of studies on alcohol and drugs, 84(1), 79–88. https://doi.org/10.15288/jsad.21-00440
Bertholet, N., Saitz, R., Hahn, J. A., Heeren, T. C., Emenyonu, N. I., Freiberg, M., Winter, M. R., Kim, T. W., Magane, K. M., Lloyd-Travaglini, C., Fatch, R., Bryant, K., Forman, L. S., Rateau, L., Blokhina, E., Muyindike, W. R., Gnatienko, N., & Samet, J. H. (2023). Impact of alcohol use disorder severity on human immunodeficiency virus (HIV) viral suppression and CD4 count in three international cohorts of people with HIV. Alcoholism, clinical and experimental research, 10.1111/acer.15031. Advance online publication. https://doi.org/10.1111/acer.15031
Tjilos, M., Tamlyn, A. L., Ragan, E. J., Assoumou, S. A., Barnett, K. G., Martin, P., Perkins, R. B., Linas, B. P., & Drainoni, M. L. (2023). "Community members have more impact on their neighbors than celebrities": leveraging community partnerships to build COVID-19 vaccine confidence. BMC public health, 23(1), 350. https://doi.org/10.1186/s12889-023-15198-6
Alrawashdeh, M., Rhee, C., Klompas, M., Larochelle, M. R., Poland, R. E., Guy, J. S., & Kimmel, S. D. (2023). Association of Early Opioid Withdrawal Treatment Strategy and Patient-Directed Discharge Among Hospitalized Patients with Opioid Use Disorder. Journal of general internal medicine, 10.1007/s11606-023-08059-w. Advance online publication. https://doi.org/10.1007/s11606-023-08059-w
Chandler, R., Nunes, E. V., Tan, S., Freeman, P. R., Walley, A. Y., Lofwall, M., Oga, E., Glasgow, L., Brown, J. L., Fanucchi, L., Beers, D., Hunt, T., Bowers-Sword, R., Roeber, C., Baker, T., & Winhusen, T. J. (2023). Community selected strategies to reduce opioid-related overdose deaths in the HEALing (Helping to End Addiction Long-term SM) communities study. Drug and alcohol dependence, 245, 109804. Advance online publication. https://doi.org/10.1016/j.drugalcdep.2023.109804
Romero-Rodríguez, E., Fuster, D., Pérula de Torres, L. Á., & Saitz, R. (2023). Is clinicians' alcohol consumption associated with their preventive practices to reduce unhealthy alcohol use? A systematic review of current evidence. Alcoholism, clinical and experimental research, 47(1), 7–17. https://doi.org/10.1111/acer.14962
Sabharwal, V., Demos, R., Snyder-Cappione, J., Parker, S. E., Shaik-Dasthagirisaheb, Y., Hunnewell, J., Boateng, J., Clarke, K., Yuen, R., Barnett, E., Yarrington, C., Taglauer, E., & Wachman, E. M. (2023). Cytokine levels in maternal and infant blood after COVID-19 vaccination during pregnancy in comparison with unvaccinated controls. Journal of reproductive immunology, 156, 103821. Advance online publication. https://doi.org/10.1016/j.jri.2023.103821
 en
en 

 Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español Tiếng Việt
Tiếng Việt Kreyol ayisyen
Kreyol ayisyen