Parents should raise concerns about their child’s behavior and development to their child’s pediatrician or healthcare provider. Children should have developmental surveillance done by their healthcare provider at every well child visit. Your child’s healthcare provider should look for any delays in development or social interaction.
There are several “red flags” for ASDs that you and your child’s healthcare provider can look for, such as if the child:
- does not babble or coo by 12 months of age
- does not gesture (point, wave, grasp, etc.) by 12 months of age
- does not say any single words by 16 months of age
- does not say two word phrases on his or her own by 24 months of age
- has ANY loss of ANY language or social skill at ANY age
Evaluation
The evaluation of a child with signs or symptoms of ASDs should be done by an autism specialist who has expertise in caring for children with ASDs. This can be a pediatric neurologist, a developmental/behavioral pediatrician, or a child psychiatrist. The autism specialist may enlist other professionals to assist with the evaluation and treatment plan for your child. These professionals may include speech and language therapists, occupational therapists, physical therapists, and child psychologists. Other professionals who may also be involved in developing a treatment plan for your child include people with expertise in certain autism specific therapies, such as Applied Behavior Analysis (ABA), Floortime, and TEACCH.
Children undergoing an evaluation should have comprehensive testing of their speech, language, and communication skills, their cognitive (problem solving) skills, and their academic skills (if children are school aged). Typically, blood is drawn to test for the known genetic causes of ASDs.
EEG Routine
Children with developmental delay or autism are at higher risk for seizures. Your doctor may recommend an EEG if there are signs of seizures such as staring or twitching.
EEG stands for electroencephalogram. An EEG is able to record information about the brain's electrical activity. During an EEG, electrodes are pasted to the scalp. The electrodes have wires that attach to a special computer that detects electrical activity coming from brain.
EEGs may be recorded in an outpatient laboratory, at home, or in the hospital. Your doctor will determine the best setting for your child.
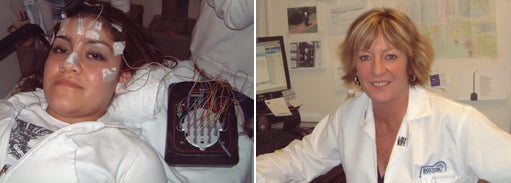
Left: Electrodes are pasted and taped. Right: Mary Russo, Supervisor of Neurophysiology at Boston Medical Center says, "Parents should bring along things from home that are comforting to their child."
Preparing for your child's EEG
Having an EEG can be a frightening experience for some children. To make the process as comfortable as possible, experts recommend bringing along your child's pillow, favorite blanket, or stuffed animal to the test.
- Children less than 2 years of age: wake the child up two hours earlier than usual in the morning and do not allow a nap the day of the EEG
- Children 2-6 years of age: keep the child up two hours later than usual and wake them at 6:00 AM; do not allow napping before the EEG
- Children 6 years or older: keep the child up until 11:00 PM -12:00 AM the night before the EEG; wake them at 5:00 AM - 6:00 AM the day of the test
If you need to drive to the medical center for the EEG, it is helpful to take along another adult to help keep your child awake and prevent napping in the car.
If your child has a love object for sleep, such as a blanket or stuffed animal, please take it along for the study.
Infants may be soothed by nursing or bottle feeding. If you give your baby a bottle, please bring one along.
If you shampoo your child's hair before the study, use only shampoo without conditioner, oil, creams, or gels. Hair should be left loose, no beads or braids.
On the day of the test, your child may eat normally but avoid food or drinks with caffeine such as hot chocolate, tea, or soda. If your child drinks from a bottle, please bring one with you.
If your child takes a stimulant (medication used for attention deficit disorder such as methylphenidate or dexedrine), ask your physician if it should not be given on the day of the EEG. All other medications should be given as prescribed.
Do not take other young children with you to the EEG lab. It is important that the lab be a quiet place to promote sleeping.
Once at the EEG lab, your child will need to lie down on a stretcher. The EEG technician will paste little metal discs called electrodes to his/her head. This does not hurt, but sometimes the children do not like holding still. The lights will be turned low to help promote sleep.
During the EEG, a few techniques are used to help see abnormal electrical activity easier. Bright lights may be flashed on and off for a few seconds.
Older children will be asked to breathe deeply for a few minutes.
Once the EEG is complete, the technician will remove the electrodes and paste. Shampoo and conditioner will take out any leftover paste.
Video EEG Monitoring
Children with developmental delay or autism are at higher risk for seizures. Your doctor may recommend an EEG if there are signs of seizures such as staring or twitching.
Video EEG monitoring (also called Long Term Monitoring or LTM) continuously records the brain's electrical activity with an EEG while simultaneously recording a movie of the patient with a videocamera. The testing may last hours to days. This procedure can be done at home, but is more commonly done in the hospital. The goal of video EEG monitoring is to record the clinical and electrical expression of a seizure. It is the gold standard for diagnosing seizures.
Video EEG is recommended when:
- spells are frequent
- it is not clear the events are seizures
- the seizure type/s are uncertain
- seizures are refractory (seizures that are difficult to treat)
- seizure frequency is uncertain, especially when seizures are subtle
- the density of seizure discharges in sleep needs to be recorded, and
- there has been a change in mental status
Preparing for your child's video EEG Long Term Monitoring usually involves an admission to the hospital for one to five days to record on videocamera and EEG some of the seizure spells a child is having.
It is crucial that an adult who has seen the spells or seizures stay with your child. Usually, children come with a parent or guardian. The parent or guardian must stay with their child continuously during the study, as they will need to push a button on the computer every time a seizure spell is witnessed or suspected. Also the parent will be asked to keep a log of seizure activity. Parents will need to write down the symptoms of the seizure and the time that the seizure began and stopped.
Usually, a foldout sleep chair and meals are provided for one parent or guardian. It may be helpful to make a plan with another adult who knows the child well to take turns staying overnight.
The EEG wires are glued on the child's head and then wrapped in gauze to help keep them in place. The EEG technicians refresh the electrodes' glue every 24 hours.

It is important for your child to stay in view of the camera. For older children we try to limit activities to the bed. It is important that parents, nurses, and doctors do not stand in the way of the camera. Your child will have bathroom access and privacy.
We recommend bringing books, video games, movies, homework, and games that will help pass the time and entertain your child. You may also bring a pillow or blanket to make your child more comfortable. At some facilities, a child life therapist will meet with you and your child upon admission to provide activities for diversion.
Your child should wear clothing or pajamas that are comfortable. A top that buttons down the front is recommended, as it will be difficult to take clothing over the head once the EEG is connected.
There may be some residual glue left in the hair after the study is completed. It is best removed by first applying baby oil or hair conditioner to the clumps and scalp for 15 minutes prior to shampoo. Then shampoo, recondition, and gently comb out using wide tooth comb.
Please bring all your child's medicines with you. Also it is helpful to bring a list of past seizure medicines and doses your child may have been on with the reason why it was stopped.
CT Scan and MRI
CT scan
A CT (Computerized Tomography) scan or CAT scan is an X-ray of the brain and bones in the skull. It can identify substantial problems in the brain such as large tumors or bleeding but is not very good for seeing the brain's fine details.
MRI
MRI (Magnetic Resonance Imaging) uses radiofrequency waves and a strong magnetic field rather than X-rays to provide a clear and detailed picture of the brain.

Left: Katie, a child life specialist at Boston Medical Center, with 12 year old, Cody, explaining the MRI procedure. Right: Heather, a pediatric sedation nurse, with 12 year old Cody. Cody was able to lie still for his MRI without medication.
Sleep Evaluation
Sleep is very important for keeping our bodies healthy. When we do not sleep well, our brains do not function well. There are many reasons why children do not sleep well. Talk to your doctor if you suspect sleep is a problem for your child.
Sleep Disorders
The three most common childhood sleep disorders are insomnia, hypersomnia, and parasomnia.
- Insomnia may include difficulties falling asleep or staying asleep.
- Hypersomnia includes narcolepsy, altered sleep patterns (circadian rhythm disorders), obstructive sleep apnea, and Kleine Levin syndrome
- Parasomnia includes confusion after awakening, sleepwalking, sleep talking, night terrors, nightmares, periodic limb movements in sleep (restless leg syndrome), and benign sleep myoclonus.
Sleep difficulties are more often seen in children with neurological problems, including epilepsy, autistic spectrum disorders, developmental disorders, hypotonia, cerebral palsy, attention deficit disorders, mood disorders, and movement disorders, including tics. They are also seen in a number of non-neurological disorders, including obesity, breathing disorders, and structural disorders of ears, mouth, and throat.
For an appointment for sleep evaluation at the Boston Medical Center, please call 617.414.5728.
Genetic Testing for Autism
In many cases, autism and developmental delay may have a genetic origin. Therefore, genetic testing may be helpful to explain the underlying science of your child's disorder. A clinical genetics evaluation in concert with genetic testing is frequently beneficial to identify an underlying and unifying diagnosis.
As new genetic tests and methods become frequently available, continued follow-up and reevaluation by geneticists remains important. The goal of genetic testing is to establish a specific diagnosis so that better guidance, treatment, and support may be provided.
In some cases, more accurate genetic recurrence risk counseling, carrier testing, and future prenatal diagnosis may be available.
For an appointment for genetic evaluation/counseling at the Boston Medical Center, please call 617.638.5106.
 en
en 
 Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español Tiếng Việt
Tiếng Việt Kreyol ayisyen
Kreyol ayisyen