A common cause of low back and leg pain is lumbar spinal stenosis.
As we age, our spines change. These normal wear-and-tear effects of aging can lead to narrowing of the spinal canal. This condition is called spinal stenosis. Spinal stenosis occurs when the space around the spinal cord narrows. This puts pressure on the spinal cord and the spinal nerve roots, and may cause pain, numbness, or weakness in the legs.
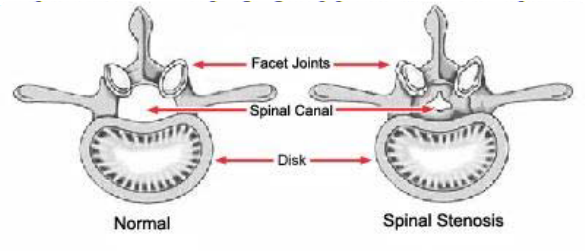
This illustration shows a healthy vertebra and a vertebra with narrowing of the spinal canal, called stenosis.
Degenerative changes of the spine are seen in up to 95% of people by the age of 50. Spinal stenosis most often occurs in adults over 60 years old. Pressure on the nerve roots is equally common in men and women.
A small number of people are born with back problems that develop into lumbar spinal stenosis. This is known as congenital spinal stenosis. It occurs most often in men. People usually first notice symptoms between the ages of 30 and 50.
What is the anatomy of the spine?
Your spine is made up of small bones, called vertebrae, which are stacked on top of one another. Muscles, ligaments, nerves, and intervertebral discs are additional parts of your spine.
What causes spinal stenosis?
Arthritis is the most common cause of spinal stenosis. Arthritis refers to the breakdown of any joint in the body.
In the spine, arthritis can result as the disc breaks down and loses water content. In children and young adults, discs have high water content. As we get older, our discs begin to dry out and weaken. This problem causes settling, or collapse, of the disc spaces and loss of disc space height.
As the spine settles, two things occur. First, weight is transferred to the facet joints. Second, the tunnels that the nerves exit through become smaller.
As the joints experience increased pressure, they also begin to degenerate and develop arthritis, similar to that occurring in the hip or knee joint. The cartilage that covers and protects the joints wears away. If the cartilage wears away completely, it can result in bone rubbing on bone.
To make up for the lost cartilage, your body may respond by growing new bone in your facet joints to help support the vertebrae. Over time, this bone overgrowth-called spurs- may narrow the space for the nerves to pass through.
Also, when arthritis develops in the lower back, ligaments around the joints increase in size meaning there is even less space for the nerves. Once the space has become small enough to irritate spinal nerves, this is what causes the pain.
What are symptoms of spinal stenosis?
Back pain. People with spinal stenosis `may or may not have back pain, depending on the degree of arthritis that has developed.
Burning pain in buttocks or legs (sciatica). Pressure on spinal nerves can result in pain in the areas that the nerves supply. The pain may be described as an ache or a burning feeling. It typically starts in the area of the buttocks and radiates down the leg. As it progresses, it can result in pain in the foot.
Numbness or tingling in buttocks or legs. As pressure on the nerve increases, numbness and tingling often accompany the burning pain. Although not all patients will have both burning pain and numbness and tingling.
Weakness in the legs or "foot drop." Once the pressure reaches a critical level, weakness can occur in one or both legs. Some patients will have a foot-drop, or the feeling that their foot slaps on the ground while walking.
Less pain with leaning forward or sitting. Studies of the lumbar spine show that leaning forward can actually increase the space available for the nerves. Many patients may note relief when leaning forward and especially with sitting. Pain is usually made worse by standing up straight and walking. Some patients note that they can ride a stationary bike or walk leaning on a shopping cart. Walking more than 1 or 2 blocks, however, may bring on severe sciatica or weakness.
How is a spinal stenosis diagnosed?
After discussing your symptoms and medical history, your doctor will examine your back. This will include looking at your back and pushing on different areas to see if it hurts.
Your doctor may have you bend forward, backward, and side-to-side to look for limitations or pain.
Spinal Stenosis Imaging Tests
Other tests which may help your doctor confirm your diagnosis include:
X-rays. Although they only visualize bones, X-rays can help determine if you have spinal stenosis. X-rays will show aging changes, like loss of disc height or bone spurs. X-rays taken while you lean forward and backward can show "instability" in your joints. X-rays can also show too much mobility. This is called spondylolisthesis.
Magnetic resonance imaging (MRI). This study can create better images of soft tissues, such as muscles, discs, nerves, and the spinal cord.
Additional tests. Computed tomography (CT) scans can create cross-section images of your spine. Your doctor may also order a myelogram. In this procedure, dye is injected into the spine to make the nerves show up more clearly. It can help your doctor determine whether the nerves are being compressed.
How is a spinal stenosis treated without surgery?
Nonsurgical treatments can help restore some function and relieve pain. Although nonsurgical methods do not improve the narrowing of the spinal canal, many people report that these treatments do help relieve symptoms.
Physical therapy. Stretching exercises, massage, and lumbar and abdominal strengthening often help manage symptoms.
Anti-inflammatory medications. Because stenosis pain is caused by pressure on a spinal nerve, reducing inflammation (swelling) around the nerve may relieve pain. Non-steroidal anti-inflammatory drugs (NSAIDs) initially provide pain relief. When used over the course of 5-10 days, they can also have an anti-inflammatory effect.
Steroid injections. Cortisone is a powerful anti-inflammatory drug. Cortisone injections around the nerves or in the "epidural space" can decrease swelling, as well as pain. They also reduce numbness, but not weakness, in the legs. Patients should receive no more than three injections a year.
Acupuncture. Acupuncture can be helpful in treating some of the pain for less severe cases of lumbar stenosis. Although it can be very safe, long-term success with this treatment has not been proven scientifically.
Chiropractic manipulation. Chiropractic manipulation is generally safe and can help with some of the pain from lumbar stenosis. Care should be taken if a patient has osteoporosis or disc herniation. Manipulation of the spine in these cases can worsen symptoms or cause other injuries.
How is a spinal stenosis treated with surgery?
If nonsurgical treatment does not work, surgery may be recommended.
Surgery for lumbar spinal stenosis is generally reserved for patients who have poor quality of life due to pain and weakness. Patients may complain of difficulty walking for extended periods of time. This is often the reason that patients consider surgery.
There are two main surgical options to treat lumbar spinal stenosis: laminectomy and spinal fusion. Both options can result in excellent pain relief. Be sure to discuss the advantages and disadvantages of both with your doctor.
What is a laminectomy?
Laminectomy involves removing the bone, bone spurs, and ligaments that are compressing the nerves. This procedure may also be called a "decompression."
Laminectomy can be performed as open surgery, in which your doctor uses a single, larger incision to access your spine. The procedure can also be done using a minimally invasive method, where several smaller incisions are made. Your doctor will discuss the best option for you.
What is spinal fusion?
If arthritis has progressed to spinal instability, a combination of decompression and stabilization or spinal fusion may be recommended.
What is the recovery like for spinal stenosis surgery?
After surgery, you may stay in the hospital for a short time, depending on your health and the procedure performed. Healthy patients who undergo just decompression may go home the same or next day, and may return to normal activities after only a few weeks. Fusion generally adds 2 to 3 days to the hospital stay.
Your surgeon may give you a brace or corset to wear for comfort. He or she will likely encourage you to begin walking as soon as possible. Most patients only need physical therapy to strengthen their backs.
Your physical therapist may show you exercises to help you build and maintain strength, endurance, and flexibility for spinal stability. Some of these exercises will help strengthen your abdominal muscles, which help support your back. Your physical therapist will create an individualized program, taking into consideration your health and history.
Most people can go back to a desk job within a few days to a few weeks after surgery. They may return to normal activities after 2 to 3 months. Older patients who need more care and assistance may be transferred from the hospital to a rehabilitation facility prior to going home.
What are the risks of spinal stenosis surgery?
There are minor risks associated with every surgical procedure. These include bleeding, infection, blood clots, and reaction to anesthesia. These risks are usually very low.
Elderly patients have higher rates of complications from surgery. So do overweight patients, diabetics, smokers, and patients with multiple medical problems.
Specific complications from surgery for spinal stenosis include:
- Tear of the sac covering the nerves (dural tear)
- Failure of the bone fusion to heal
- Failure of screws or rods
- Nerve injury
- Need for further surgery
- Failure to relieve symptoms
- Return of symptoms
How successful is spinal stenosis surgery?
Overall, the results of laminectomy with or without spinal fusion for stenosis are good to excellent in the majority of patients. Patients tend to see more improvement of leg pain than back pain. Most patients are able to resume a normal lifestyle after a period of recovery from surgery.
Departments and Programs Who Treat This Condition
Orthopedic Surgery
 en
en 
 Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español Tiếng Việt
Tiếng Việt Kreyol ayisyen
Kreyol ayisyen