In spondylolisthesis, one of the bones in your spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar spine). In some people, this causes no symptoms at all. Others may have back and leg pain that ranges from mild to severe.
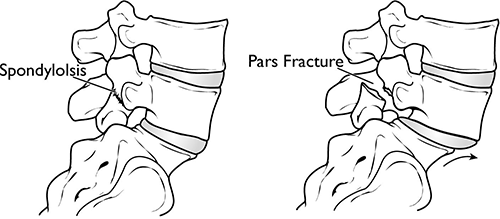
(Left) In spondylolysis, a fracture often occurs at the pars interarticularis. (Right) Because of the pars fracture, only the front part of the bone slips forward.
What are the different types of spondylolisthesis?
Many types of spondylolisthesis can affect adults. The two most common types are degenerative and spondylolytic. There are other less common types of spondylolisthesis, such as slippage caused by a recent, severe fracture or a tumor.
What is degenerative spondylolisthesis?
As we age, general wear and tear causes changes in the spine. Intervertebral discs begin to dry out and weaken. They lose height, become stiff, and begin to bulge. This disc degeneration is the start to both arthritis and degenerative spondylolisthesis (DS).
As arthritis develops, it weakens the joints and ligaments that hold your vertebrae in the proper position. The ligament along the back of your spine (ligamentum flavum) may begin to buckle. One of the vertebrae on either side of a worn, flattened disc can loosen and move forward over the vertebra below it. This can narrow the spinal canal and put pressure on the spinal cord. This narrowing of the spinal canal is called spinal stenosis and is a common problem in patients with DS.
Women are more likely than men to have DS, and it is more common in patients who are older than 50. A higher incidence has been noted in the African-American population.
What is spondylolytic spondylolisthesis?
One of the bones in your lower back can break and this can cause a vertebra to slip forward. The break most often occurs in the area of your lumbar spine called the pars interarticularis.
In most cases of spondylolytic spondylolisthesis, the pars fracture occurs during adolescence and goes unnoticed until adulthood. The normal disc degeneration that occurs in adulthood can then stress the pars fracture and cause the vertebra to slip forward. This type of spondylolisthesis is most often seen in middle-aged men.
Because a pars fracture causes the front (vertebra) and back (lamina) parts of the spinal bone to disconnect, only the front part slips forward. This means that narrowing of the spinal canal is less likely than in other kinds of spondylolisthesis, such as DS in which the entire spinal bone slips forward.
What are the symptoms of degenerative spondylolisthesis?
Patients with DS often visit the doctor's office once the slippage has begun to put pressure on the spinal nerves. Although the doctor may find arthritis in the spine, the symptoms of DS are typically the same as symptoms of spinal stenosis. For example, DS patients often develop leg and/or lower back pain. The most common symptoms in the legs include a feeling of vague weakness associated with prolonged standing or walking.
Leg symptoms may be accompanied by numbness, tingling, and/or pain that is often affected by posture. Forward bending or sitting often relieves the symptoms because it opens up space in the spinal canal. Standing or walking often increases symptoms.
What are the symptoms of spondylolytic spondylolisthesis?
Most patients with spondylolytic spondylolisthesis do not have pain and are often surprised to find they have the slippage when they see it in x-rays. They typically visit a doctor with low back pain related to activities. The back pain is sometimes accompanied by leg pain.
How is a spondylolisthesis diagnosed?
Doctors diagnose both DS and spondylolytic spondylolisthesis using the same examination tools.
After discussing your symptoms and medical history, your doctor will examine your back. This will include looking at your back and pushing on different areas to see if it hurts. Your doctor may have you bend forward, backward, and side- to-side to look for limitations or pain.
Other tests which may help your doctor confirm your diagnosis include:
X-rays. These tests visualize bones and will show whether a lumbar vertebra has slipped forward. X-rays will show aging changes, like loss of disc height or bone spurs. X-rays taken while you lean forward and backward are called flexion-extension images. They can show instability or too much movement in your spine.
Magnetic resonance imaging (MRI). This study can create better images of soft tissues, such as muscles, discs, nerves, and the spinal cord. It can show more detail of the slippage and whether any of the nerves are pinched.
Computed tomography (CT). These scans are more detailed than x-rays and can create cross-section images of your spine.
How is spondylolisthesis treated without surgery?
Although nonsurgical treatments will not repair the slippage, many patients report that these methods do help relieve symptoms.
Physical therapy and exercise. Specific exercises can strengthen and stretch your lower back and abdominal muscles.
Medication. Pain killers and non-steroidal anti-inflammatory medicines may relieve pain.
Steroid injections. Cortisone is a powerful anti-inflammatory. Cortisone injections around the nerves or in the "epidural space" can decrease swelling, as well as pain. It is not recommended to receive these, however, more than three times per year. These injections are more likely to decrease pain and numbness, but will not relieve weakness of the legs.
When should someone with degenerative spondylolisthesis be treated with surgery?
Patients should consider surgery for degenerative spondylolisthesis if they have tried the nonsurgical treatments for 3 to 6 months with no improvement.
Before committing to surgery, your provider will take a close look at the extent of the arthritis in your spine and whether your spine has excessive movement.
DS patients who are candidates for surgery are usually not able to walk or stand, and have a poor quality of life due to the pain and weakness.
When should someone with spondylolytic spondylolisthesis be treated with surgery?
Patients should consider surgery for spondylolytic spondylolisthesis if they have tried the nonsurgical treatments for at least 6 to 12 months with no improvement.
If the slippage is getting worse or the patient has progressive neurologic symptoms, such as weakness, numbness, or falling, and/or symptoms of cauda equina syndrome, surgery may help.
How is spondylolisthesis treated with surgery?
Surgery for both DS and spondylolytic spondylolisthesis includes removing the pressure from the nerves and spinal fusion.
Removing the pressure involves opening up the spinal canal. This procedure is called a laminectomy. Spinal fusion is essentially a "welding" process. The basic idea is to fuse together the painful vertebrae so that they heal into a single, solid bone.
Departments and Programs Who Treat This Condition
Orthopedic Surgery
Neurosurgical Spine Surgery
Spine Surgery
Musculoskeletal Medicine and Pain Management Program
 en
en 
 Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español Tiếng Việt
Tiếng Việt Kreyol ayisyen
Kreyol ayisyen