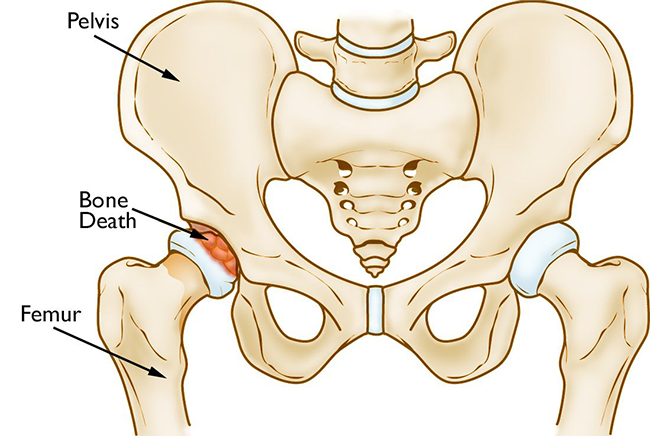
In osteonecrosis, the bone in the head of the femur slowly dies.
Osteonecrosis of the hip is a painful condition that occurs when the blood supply to the head of the femur (thighbone) is disrupted. Because bone cells need a steady supply of blood to stay healthy, osteonecrosis can ultimately lead to destruction of the hip joint and severe arthritis.
Osteonecrosis is also called avascular necrosis (AVN) or aseptic necrosis. Although it can occur in any bone, osteonecrosis most often affects the hip. More than 20,000 people each year enter hospitals for treatment of osteonecrosis of the hip. In many cases, both hips are affected by the disease.
What is the anatomy of the hip?
The hip is one of the body's largest joints. It is a "ball-and-socket" joint. The socket is formed by the acetabulum, which is a part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
The bone surfaces of the ball and socket are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones and enables them to move easily.
What causes osteonecrosis?
Osteonecrosis of the hip develops when the blood supply to the femoral head is disrupted. Without adequate nourishment, the bone in the head of the femur dies and gradually collapses. As a result, the articular cartilage covering the hip bones also collapses, leading to disabling arthritis.
Osteonecrosis can affect anyone, but is more common in people between the ages of 40 and 65. Men develop osteonecrosis of the hip more often than women.
Who is at risk of developing osteonecrosis?
It is not always known what causes the lack of blood supply, but providers have identified a number of risk factors that can make someone more likely to develop osteonecrosis:
- Injury. Hip dislocations, hip fractures, and other injuries to the hip can damage the blood vessels and impair circulation to the femoral head.
- Excessive alcohol use. Overconsumption of alcohol over time can cause fatty deposits to form in the blood vessels and can elevate cortisone levels, resulting in a decreased blood supply to the bone.
- Corticosteroid medicines. Many diseases, including asthma, rheumatoid arthritis, and systemic lupus erythematosus, are treated with steroid medications. Although it is not known exactly why these medications can lead to osteonecrosis, research shows that there is a connection between the disease and long-term corticosteroid use.
- Medical conditions. Osteonecrosis is associated with other diseases, including Caisson disease (diver's disease or "the bends"), sickle cell disease, myeloproliferative disorders, Gaucher's disease, systemic lupus erythematosus, Crohn's disease, arterial embolism, thrombosis, and vasculitis.
What are symptoms of osteonecrosis?
Osteonecrosis develops in stages. Hip pain is typically the first symptom. This may lead to a dull ache or throbbing pain in the groin or buttock area. As the disease progresses, it becomes more difficult to stand and put weight on the affected hip, and moving the hip joint is painful.
It may take from several months to over a year for osteonecrosis to progress. It is important to diagnose osteonecrosis early, because some studies show that early treatment is associated with better outcomes
How is osteonecrosis diagnosed?
After discussing your symptoms and medical history, your provider will examine your hip to discover which specific motions cause your pain.
Patients with osteonecrosis often have severe pain in the hip joint but relatively good range of motion. This is because only the femoral head is involved in the earlier stages of the disease. Later, as the surface of the femoral head collapses, the entire joint becomes arthritic. Loss of motion and stiffness can then develop.
Diagnostic Tests
This test uses a magnetic field, radiofrequency pulses, and a computer to produce detailed images of body structures in multiple places. You may be asked to drink a contrast solution for better imaging, and you will most likely lie on a moving table as pictures are taken.
Magnetic Resonance Imaging (MRI)A form of electromagnetic radiation with very high frequency and energy. X-rays are used to examine and make images of things such as the bones and organs inside the body.
X-RaysDepartments and Programs Who Treat This Condition
Orthopedic Surgery
Hip and Knee Arthroplasty (Replacement)
Musculoskeletal Medicine and Pain Management Program
Hip Preservation
 en
en 
 Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español Tiếng Việt
Tiếng Việt Kreyol ayisyen
Kreyol ayisyen