
Rewriting healthcare means providing all patients access to the best possible therapies.
Rewriting Healthcare by Fabio Petrocca, MD, director of the CAR T-cell Therapy Program
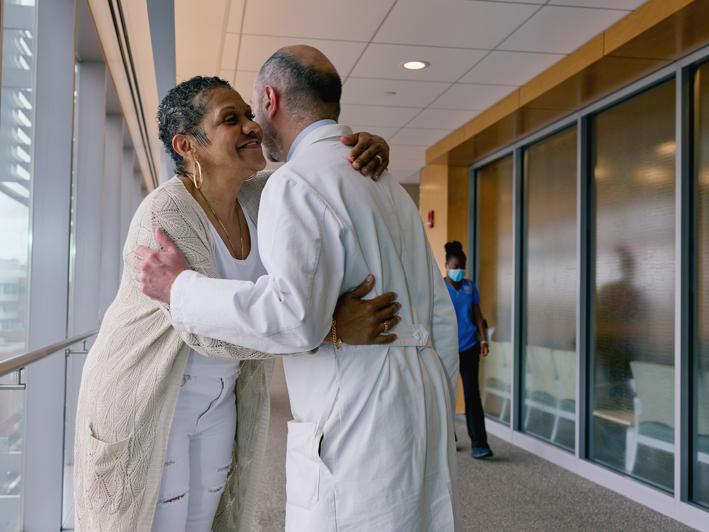
Physician-scientist Dr. Fabio Petrocca is a world-renowned expert on CAR (chimeric antigen receptor) T-cell therapy (CAR T). This innovative, one-time treatment uses genetically engineered versions of a patient’s own immune cells to combat tough-to-treat cancers. Dr. Petrocca was involved in the development of CAR T and saw what a huge difference the treatment made for patients who had access to it. “As the next step in my career, it made sense to try to solve another important problem related to these therapies — patient access. And that is really what motivated me to come to BMC.”
As director of the CAR T-cell Therapy Program at Boston Medical Center, Dr. Petrocca has brought this lifesaving therapy to patients who might not otherwise have access to it. “It has been both personally and professionally very rewarding to see this is something we can do at BMC,” he says.
Learn how Dr. Petrocca and BMC are rewriting healthcare by offering the latest treatments for cancer to all patients.
What did it take to bring CAR T-cell therapy to BMC?
We started working on the CAR T program here at BMC about two years ago, and we officially launched in August 2022. Bringing these complex therapies to patients is not trivial. CAR T remains a very complicated procedure that requires a lot of different people and capabilities. We had to make sure we had the right people, the right training, and the right clinical infrastructure in place to deliver CAR T safely and effectively. It’s been a team effort for sure.
CAR T therapy by definition is an integrated procedure that requires expertise from hematologists, cardiologists, neurologists, and nephrologists. And that’s been one of our biggest achievements to date — that we’ve been able to build such an experienced team across very different disciplines focused on CAR T.
It was also important that we had everything we needed in the same building, allowing us to rapidly respond to any complication that could be associated with CAR T-cell therapy. We’re blessed that the intensive care unit (ICU) is in the same building where CAR T-cell therapy is delivered, so we always have an ICU bed available if needed. We have the best possible support from that standpoint.
At this point, we’re fully operational, and we’re currently accepting patients. We have started treating patients with CAR T, which has been an important milestone for the program because it validates our efforts so far and, most importantly, really addresses the problem that we’ve been trying to solve. We’re very happy about where we are today, and it’s something that will continue to evolve and improve.
Why is it important that BMC now offers CAR T-cell therapy to patients?
CAR T-cell therapy is one of the most complex treatments for cancer currently available. It’s been around for about six years, so it’s not necessarily a new therapeutic modality. But CAR T is notoriously one of the most-expensive cancer treatments available, so there has been a lot of discussion in the field about whether this is a sustainable cost for the system, especially when it comes to a disadvantaged patient population that may or may not have access to commercial insurance.
The importance of the CAR T-cell Therapy Program here at BMC is that we can finally offer a new type of treatment for cancer that was not previously available to many of our patients.
What we’ve been able to build here is a path toward access to these costly therapies regardless of socioeconomic status or insurance coverage.
What we’ve been able to build here is a path toward access to these costly therapies regardless of socioeconomic status or insurance coverage.
How is BMC pushing the boundaries of cancer treatment?
When I joined BMC, what I found was a group of people that has always been motivated by challenges.
In building the clinical infrastructure to deliver these therapies to our patients, we have shown that, in fact, there is really no reason why these therapies should not be available to all patients. We’re very proud of this achievement, and we hope that we can serve as a model for other institutions in the U.S. and elsewhere to support the use of these therapies in many different contexts, not just in certain large academic hospitals.
Our program is an integrated clinical research program, meaning that our patients have access to currently available T-cell therapies, but there is also a strong emphasis on facilitating access to clinical trials of newer CAR T-cell therapies that may be even better than the current ones.

What does “rewriting health care” mean to you?
Rewriting healthcare comes down to building access to novel therapies for patients who traditionally would not have access to these therapies.
How is BMC rewriting health care?
BMC provides the best possible care to all patients, regardless of their personal circumstances. Traditionally, CAR T has been considered one of the most complex procedures, and the assumption has always been that there are only certain hospitals that can provide these therapies effectively. At BMC, we have been challenging this dogma. It took a while to convince everyone that this is something that would be feasible, and eventually we got there. Now there is much more confidence that this is a treatment that can and should be available to patients at BMC and similar institutions.




