The Center for Voice and Swallowing offers a wide range of services and specialty care for adults and feeding therapy for children. We team up with many disciplines to make sure we are providing a team-based approach to giving you the best treatment possible. Our goal is to deliver high quality care to all of our patients.
Our team of Speech Language Pathologists are trained as specialists in many areas. We treat voice, swallowing, breathing, language, speech problems, and many other issues related to Speech Language Pathology. We can provide services at many different levels of care, ranging from acute problems (for those who need to be seen during an inpatient stay) to ongoing, chronic problems (for those who can be seen in our clinic). Based on a philosophy of using evidence-based practice, team work, and patient-centered approaches, we hope that our comprehensive care will empower our patients through rehabilitation.
To schedule a consult with one of BMC’s speech language pathologists, call us at 617.638.8124.
Telehealth Visits
At the Voice and Swallowing Center, we recognize that COVID-19 continues to be challenging for so many of our patients. But we want you to know that we’re still here for you.
We offer virtual health visits for voice and swallowing therapy through your phone, tablet, or computer. While you stay in the comfort of your own home, we can provide you with:
- Assistance with breathing issues
- Troubleshooting for issues with your tracheo-esophageal prosthesis (TEP, aka voice prosthesis)
- Assistance with diet modifications
- Check ins on swallowing exercises
- Real-time exercises for voice issues, globus syndrome, and swallowing
- Breathing courses for Long COVID symptoms
To schedule an appointment, call 617.638.8124. You can also find out more about telehealth at BMC here.
Contact Us
Ground Flooor, Suite 1400
Moakley Building 617.638.8124
Monday-Friday - 7:30 AM - 5:00 PM
Diagnostics and Tests
- Flexible Endoscopic Evaluation of Swallowing (FEES)
- Modified Barium Swallow exams (MBS)
- Clinical Swallowing Evaluation (CSE) and Pediatric Feeding Evaluations
- Pharyngeal pH probe testing
- Pharyngeal Manometry
- Esophageal function as it relates to pharyngeal swallowing
- Adult Language Evaluations
- Adult Speech Evaluations
- Adult Articulation Evaluations
- Voice Screenings
Our Team
Jessica M. Pisegna, MS-CCC-SLP, MEd

Daniel P. Buckley, MS, CCC-SLP

Michelle G. Ganann, MS CCC-SLP

Hadas Golan, MS, CCC-SLP

Amy M. Gottlieb, MS, CCC-SLP

Edel M. McNally, MS, CCC-SLP, BCS-S

Eileen Miglio, MS, CCC-SLP

Juliet Ochura, MS, CCC-SLP, CLC

Meredith B. O'Dea, MS CCC-SLP

Kerry Pearl, MS, CCC-SLP

- Samantha Ashinoff, MS, CCC-SLP
- Kim Boscodoss, MS, CCC-SLP
- Michelle Ganann, CCC-SLP
- Anna Lifvergren, CCC-SLP
- Elona Meziu, CCC-SLP-CF 2024-2025
- Keri Miloro, CCC-SLP
- Kelly Morgan, MS, CCC-SLP
- Emily O'Gorman, MS, CCC-SLP
- Chloe Thorburn, CCC-SLP
Patient Resources
Research Overview
Our team has a strong interest in research. Our research aims to make evaluations faster, more accurate, and simpler, and we also study treatment and which methods get patients better.
Why is research important?
- A research study is a scientific way to improve or develop new methods of health care. Studies are designed to answer specific questions on how to prevent, diagnose, or treat diseases and disorders. Many types of research studies exist. For example, clinical trials test new evaluation processes to make sure we are studying the correct swallowing parts, for example. Other studies use interviews or surveys to understand health or behavior.
- Research studies are important because they help us understand knowledge and progress on diseases and disorders. Research is the fastest and safest way to find treatments that work. That’s why we value research and have multiple ongoing studies. Research helps:
- to learn about ways to possibly improve your health
- to help in the evaluation of medications, tests, or programs that may not be available outside of research
- to potentially help others
- to further knowledge of scientific research and medical care
- to ensure our clinicians are critical thinkers and constantly trying to ensure best practices
What type of research do we do?
- We are particularly interested in studying communication, feeding, speech and swallowing disorders. Some questions we are interested in studying include:
- What types of swallowing patterns can we observe on Flexible Endoscopic Evaluation of Swallowing (FEES) exams? What types of swallowing patterns can we observe on Modified Barium Swallows (MBS)? Are clinical impression different depending on the type of evaluation? We are currently doing simultaneous studies (FEES/MBS) to investigate this question.
Parameters of Instrumental Swallowing Evaluations: Describing a Diagnostic Dilemma - In stroke patients, does frequent and intensive therapy help improve outcomes? Does it avoid potential poor outcomes like feeding tubes or longer hospital stays?
- How can we best assess sensation in the throat? In particular, is there a way to best evaluate the laryngeal adductor reflex and what does this information tell us?
- How can we teach parents to feed their children in a safe way? We are interested in the thickness of liquid and how to make sure this can be carried out at home.
- Is there a relationship between certain factors in extubated patients and laryngeal sensation?
Relationship Between Laryngeal Sensation, Length of Intubation, and Aspiration in Patients with Acute Respiratory Failure
- What types of swallowing patterns can we observe on Flexible Endoscopic Evaluation of Swallowing (FEES) exams? What types of swallowing patterns can we observe on Modified Barium Swallows (MBS)? Are clinical impression different depending on the type of evaluation? We are currently doing simultaneous studies (FEES/MBS) to investigate this question.
- We also are investigating outcomes in laryngectomy patients.
- Does the size of the voice prosthesis matter?
- What types of improvements do we notice in patients who use laryngectomy tubes and heat-moisture exchange devices?
- We are also looking at voice research.
- What information can we learn from patient-reports symptoms? Are there influences like language and other socioeconomic barriers?
- What type of voice evaluation data can inform therapy, for example types of muscle tension and cepstral peak prominence? How can we best rehabilitate the professional voice?
http://sites.bu.edu/stepplab/lab-members/ - Does manual therapy help to reduce problems in patients such as breathing, tension, and anxiety?
http://www.breatheon.com/about-us/
- Improving safety for at-risk patients by providing them with an AAC (augmentative and alternative communication) via a tailored system. Boston Medical Center cares for a vulnerable population, and when our patients are admitted to the hospital, some of them are rendered even more vulnerable to serious medical outcomes due to their loss of communication abilities. By empowering these patients to use a tailored communication system regardless of their medical condition, we will demonstrate that serious medical outcomes can be prevented when patients are given the ability to communicate their wants and needs effectively. Further, we have built into our plan several action items for sustainability, allowing us to make communication an option for all admitted patients in the future. We have been awarded a 2-year grant to implement this program, entitled: "Empowering Expression Through Innovation for Patients in Acute Care."
- Our pediatric feeding team has been awarded Health Equity Accelerator Seed Funding for a project entitled: “Through Thick and Thin: Improving Health Outcomes for Children with Aspiration.” We aim to study how health inequities impact children with feeding disorders. For instance, in trying to mitigate aspiration risk, they often grapple with parents not being able to access the supplies needed for thickening the infant’s or child’s liquids when medically indicated. Our unique population of patients at Boston Medical Center, who derive from financially, racially, culturally, and socially diverse backgrounds are at higher risk for health inequities. In families who are non-English speaking, understanding the recommendations for thickening their child’s liquids becomes even more challenging. We aim to study be a positive step to helping bridge the divide for accessing necessary thickening materials. By enabling families to have the tools they need to thicken the liquids appropriately as well as the educational support to implement the instructions, we may be able to reduce hospitalizations, support continued breast-milk feeding initiatives, and empower caregivers to have success safely feeding and nourishing their children.
- The Patient Safety Grant Committee awarded our team a grant entitled Enhancement of Safe Feeding in Pediatrics at Boston Medical Center: “ESIP Initiative.” In this initiative, we aim to assess if providing a three-tiered approach to enhancing provider education, parent education, and access to feeding therapy improves patient outcomes.
- Please call our clinic at 617-638-8124 to inquire about ongoing research studies.
Publications
Our dedicated team of clinician researchers have published many scientific papers to help advance our practice and better inform clinical care. Some of our publications from previous research include:
- Kumar S, Marchina S, Langmore S, Massaro J, Palmisano J, Wang N, Searls DE, Lioutas V, Pisegna J, Wagner C, Shinde A, Schlaug G. Fostering eating after stroke (FEASt) trial for improving post-stroke dysphagia with non-invasive brain stimulation. Sci Rep. 2022 Jun 10; 12(1):9607.View Related Profiles. PMID: 35689084; PMCID: PMC9187742; DOI: 10.1038/s41598-022-14390-9;
- Sambhu M, Goh T, Golan H, Pisegna J, Noordzij JP. Evaluating the use of baclofen as adjunct treatment for muscle tension dysphonia. Am J Otolaryngol. 2022 Mar-Apr; 43(2):103309.View Related Profiles. PMID: 34896937
- Starmer HM, Arrese L, Langmore S, Ma Y, Murray J, Patterson J, Pisegna J, Roe J, Tabor-Gray L, Hutcheson K. Adaptation and Validation of the Dynamic Imaging Grade of Swallowing Toxicity for Flexible Endoscopic Evaluation of Swallowing: DIGEST-FEES. J Speech Lang Hear Res. 2021 06 04; 64(6):1802-1810.View Related Profiles. PMID: 34033498
- Plocienniczak MJ, Patel R, Pisegna J, Grillone G, Brook CD. Evaluating a Prototype Nasolaryngoscopy Hood During Aerosol-Generating Procedures in Otolaryngology. Otolaryngol Head Neck Surg. 2021 06; 164(6):1251-1256.View Related Profiles. PMID: 33228434; PMCID: PMC7686647; DOI: 10.1177/0194599820973652;
- Ganann MG, Kitila M, Patel R, Brook CD, Pisegna JM. The FEES box: A novel barrier to contain particles during aerosol-generating procedures. Am J Otolaryngol. 2021 May-Jun; 42(3):102888.View Related Profiles. PMID: 33460980; PMCID: PMC7834572; DOI: 10.1016/j.amjoto.2020.102888;
- Tadavarthi Y, Hosseini P, Reyes SE, Focht Garand KL, Pisegna JM, Pearson WG. Pilot Study of Quantitative Methods for Differentiating Pharyngeal Swallowing Mechanics by Dysphagia Etiology. Dysphagia. 2021 04; 36(2):231-241. PMID: 32410203; PMCID: PMC7666098; DOI: 10.1007/s00455-020-10123-0;
- Kim K, Pisegna JM, Kennedy S, Langmore S. Measuring Vallecular Volume on Flexible Endoscopic Evaluation of Swallowing: A Proof of Concept Study. Dysphagia. 2021 02; 36(1):96-107.View Related Profiles. PMID: 32303907
- Marchina S, Pisegna JM, Massaro JM, Langmore SE, McVey C, Wang J, Kumar S. Transcranial direct current stimulation for post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. J Neurol. 2021 Jan; 268(1):293-304.View Related Profiles. PMID: 32797300
- Pisegna JM, Langmore SE, Meyer TK, Pauloski B. Swallowing Patterns in the HNC Population: Timing of Penetration-Aspiration Events and Residue. Otolaryngol Head Neck Surg. 2020 Dec; 163(6):1232-1239.View Related Profiles. PMID: 32633196
- McNally E, Krisciunas GP, Langmore SE, Crimlisk JT, Pisegna JM, Massaro J. Oral Care Clinical Trial to Reduce Non-Intensive Care Unit, Hospital-Acquired Pneumonia: Lessons for Future Research. J Healthc Qual. 2019 Jan/Feb; 41(1):1-9. PMID: 29634593.
- Borders JC, Fink D, Levitt JE, McKeehan J, McNally E, Rubio A, Scheel R, Siner JM, Taborda SG, Vojnik R, Warner H. Relationship Between Laryngeal Sensation, Length of Intubation, and Aspiration in Patients with Acute Respiratory Failure. Dysphagia. 2019 Jan 29:1-8.
- O’Dea MB, Langmore SE, Krisciunas GP, Walsh M, Zanchetti LL, Scheel R, McNally E, Kaneoka AS, Guarino AJ, Butler SG. Effect of lidocaine on swallowing during FEES in patients with dysphagia. Annals of Otology, Rhinology & Laryngology. 2015 Jul;124(7):537-44.
- Langmore SE, Pisegna JM. Efficacy of exercises to rehabilitate dysphagia: A critique of the literature. International Journal of Speech-Language Pathology. 2015 May 4;17(3):222-9.
- Langmore SE, McCulloch TM, Krisciunas GP, Lazarus CL, Van Daele DJ, Pauloski BR, Rybin D, Doros G. Efficacy of electrical stimulation and exercise for dysphagia in patients with head and neck cancer: A randomized clinical trial. Head & neck. 2016 Apr;38(S1):E1221-31.
- Scheel, R., Pisegna, J. M., McNally, E., Noordzij, J. P., & Langmore, S. E. (2016). Endoscopic assessment of swallowing after prolonged intubation in the ICU setting. Annals of Otology, Rhinology & Laryngology, 125(1), 43-52.
- Krisciunas GP, Castellano K, McCulloch TM, Lazarus CL, Pauloski BR, Meyer TK, Graner D, Van Daele DJ, Silbergleit AK, Crujido LR, Rybin D. Impact of compliance on dysphagia rehabilitation in head and neck cancer patients: results from a multi-center clinical trial. Dysphagia. 2017 Apr 1;32(2):327-36.
- Pisegna JM, Yang S, Purcell A, Rubio A. A Mixed-Methods Study of Patient Views on Reflux Symptoms and Medication Routines. J Voice. 2017 May; 31(3):381.e15-381.e25. PMID: 27647519.
- Meyer TK, Pisegna JM, Krisciunas GP, Pauloski BR, Langmore SE. Residue influences quality of life independently of penetration and aspiration in head and neck cancer survivors. Laryngoscope. 2017 Jul; 127(7):1615-1621. PMID: 27861932.
- Kaneoka A, Pisegna JM, Saito H, Lo M, Felling K, Haga N, LaValley MP, Langmore SE. A systematic review and meta-analysis of pneumonia associated with thin liquid vs. thickened liquid intake in patients who aspirate. Clin Rehabil. 2017 Aug; 31(8):1116-1125. PMID: 28730887.
- May NH, Pisegna JM, Marchina S, Langmore SE, Kumar S, Pearson WG. Pharyngeal Swallowing Mechanics Secondary to Hemispheric Stroke. J Stroke Cerebrovasc Dis. 2017 May; 26(5):952-961. PMID: 27913200.
Residency and Fellowship Information
Speech Pathology Clinical Fellows
Boston Medical Center offers a Clinical Fellowship (CF), which is a requirement to obtain a degree in Speech Pathology. As stated by ASHA:
“The SLP CF is a mentored professional experience that begins after the completion of academic course work and clinical practicum. The goal of the CF is to allow the Clinical Fellow to transition between being a student enrolled in a communication sciences and disorders (CSD) program and being an independent provider of speech-language pathology clinical services. The purpose of the CF is to integrate and apply the knowledge from academic education and clinical training, evaluate strengths and identify limitations, develop and refine clinical skills consistent with the Scope of Practice in Speech-Language Pathology, and advance the Clinical Fellow from needing constant supervision to being an independent practitioner. The duration of the CF experience requires a minimum of 1,260 hours and a minimum of 36 weeks of full-time experience or its part-time equivalent.”
Dr. Pisegna developed the first Clinical Fellowship Program for the Speech Language Pathology department at Boston Medical Center in 2019. Now, clinical fellows are an important part of the program, where accepted master's level SLP graduates must complete a 12-month program. Previous fellows who have completed the BMC program include:
- Amy Gottlieb CCC-SLP 2019-2020
- Casey Scott CCC-SLP 2020-2021
- Krystal Radnor CCC-SLP 2020-2021
- Manisha Gore CCC-SLP 2021-2022
- Eileen Miglio CCC-SLP 2021-2022
- Miranda Capomaccio CCC-SLP-CF 2022-2023
The Fellows are fully mentored and intensive training is provided. We have taken many measures to ensure our clinical fellowship program is robust to ensure the Fellows meet their clinical goals and the supervisor’s goals in order to become an independent clinician. Our goal is to teach critical thinking. As Albert Einstein said, "education is not the learning of facts, rather it's the training of the mind to think." Below, Amy Gottlieb CCC-SLP (former BMC Fellow) and Kailey Vitale CCC-SLP mentor Manish Gore as she worked towards gaining her competency in administering a FEES exam. The Clinical Fellowship position is posted on the BMC Career website annually, as the position becomes available.
Graduate Students
We realize the importance of education in the field of Speech Pathology. This is why, as a teaching hospital, we often have speech pathology students, medical students, fellows, and interns accompany us during our clinical day. In collaboration with Boston University, we have developed a curriculum as a medical placement for Speech Language Pathology students. Our goal is to provide advanced knowledge and training for medical speech language pathology. Our team of clinicians provide weekly lectures, seminars, and hands-on learning in addition to mentorship during students’ placement at Boston Medical Center. Further, students observe patient care, when allowed by the patient, which enriches their experience.

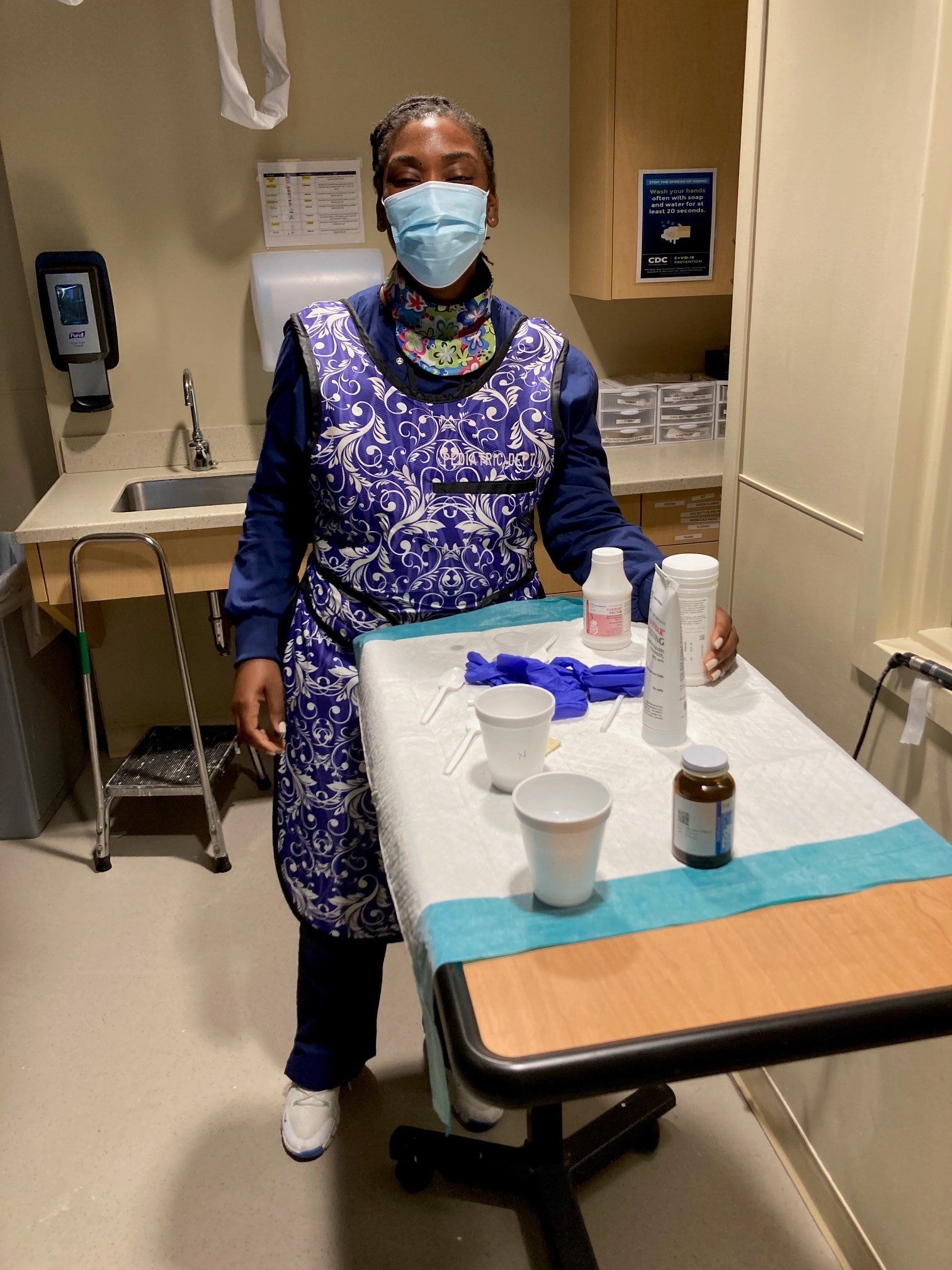
Two of our graduate students, above, during their practicum placement at BMC.
We also have welcomed students from other backgrounds. For example, Boston University’s School of Public Health Practicum Program has connected a variety of Public Health Graduate students with the Speech Pathology Department with great success. Amr Jijakli, MPH, MD published a paper with the SLPs, Anne Li MPH and Sai Chicakuragdu MPH presented at the 2023 Dysphagia Research Society in San Francisco! We feel that our graduate students make us stronger as clinicians, people, and teammates.
Mentoring and Training
Our team is also dedicated to teaching and mentoring other clinicians. Peer mentorship and training is how our clinician become competent in many of the advance skills, such as speaking valve placement, Modified Barium Swallows, and the Fiberoptic Endoscopic Evaluation of Swallowing (FEES). We also regularly hold lunch-and-learns, journal clubs, seminars, and in-services to mentor, train, and teach.
FEES was developed by Dr. Susan Langmore in 1988. FEES has become a globally recognized gold standard for evaluating oropharyngeal dysphagia and for assessing swallowing function. Dr. Langmore and her team provide two types of FEES courses at Boston University Medical Center – a two day foundation (introductory) course and a one day advanced course. Learn more. This course is not currently available.
Instagram Takeover
Tune in to see a day in the life of our Casey Scott, speech-language pathologist in the Speech-Language Pathology Department!
Casey takes us through a day in her life at BMC, introduces her team members, and shows us what it means to help patients overcome their swallowing and communication difficulties! Casey and her team also answer questions throughout the day.

