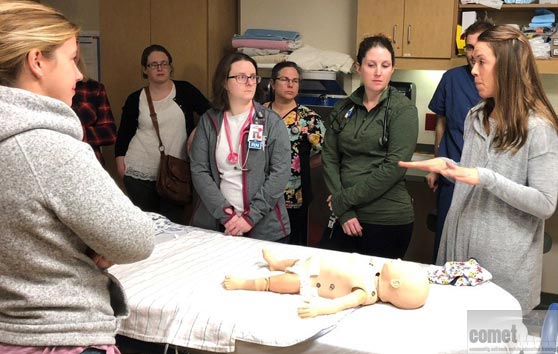
Bringing a robust, pediatric acute care simulation training program to your medical facility – anytime, anywhere for all providers to train together as a unified team!

Simulation has been shown to be effective in educating healthcare providers in medical knowledge, teamwork, systems issues identification, and patient safety. Large simulation centers at academic medical centers are truly beneficial, but not all institutions or medical facilities can afford the cost of building a state of the art simulation center. Many medical schools invite and encourage community health care providers to visit and train at their simulation center, however, finding a team of colleagues to get together and travel to a simulation center is challenging. Mobile, in-situ simulation has many advantages and is a realistic and even more beneficial training experience and is in the setting in which care providers actually work.
The COMET program aims to bridge the gaps within pediatric acute care by providing an in-situ, simulation training program to your interprofessional and interdisciplinary healthcare teams. Contact us for more information.
Benefits
- Simulation in your trauma/resuscitation room with your own equipment/room set up
- Education and medical management from content experts (MD, RN) for realistic common acute pediatric events
- Practice with institutions policies
- Systems issue identification and troubleshooting solutions
- Crisis resource management with interprofessional communication emphasis
- Discussion of latent safety threats
- Sharing of best practices and policies
- Creating longitudinal partnerships between your site and our academic center to promote bidirectional collaboration
COMET has the added convenience of creating mobile simulation programs for other disciplines. For example – we can simulate a laboring mom who delivers a premature infant in the trauma bay. This will allow resuscitation of a dual patient encounter with multiple medical issues and complex team dynamics. Please send us an inquiry and we can create scenarios for your unit.
From inpatient pediatric floor units to ambulances, the convenience of COMET is that we come to you. Read about the COMET team.
Course Structure
Programs can be tailored to meet the individual needs of each site.
Initial Session:
- 4 standard medical scenarios are run in the resuscitation bay
- Cases are validated from prior studies (see published works)
- This allows for a proper needs assessment of the department/facility
- Typical "resuscitation team" should run the scenarios – based on your unit’s typical shift staffing model (1-2 MD, 2-3 RN, 1-2 tech, 1 RRT etc.)
- Cases are common pediatric diagnoses with an infant/child presenting in a critical state requiring resuscitation
- Typically, we recommend running one "resuscitation team" through all four pediatric emergency simulation cases and then repeating all 4 case scenarios with a new team naïve to the cases
The sessions are truly flexible and modifications can be made in the format to meet the needs of each site. For example, the number of different "resuscitation teams" running each case be varied. For time constraints, this can be split into as many teams as desired.
- 1 team running 1 of 4 cases (= 4 teams total)
- 2 teams running 2 of 4 cases (= 2 teams total)
In this setting, teams would stay for all 4 cases and participate in the debrief and observation of the cases that they also do not lead or participate in. Thus, we ensure learning for all providers for each of the 4 standard scenarios. Usually, there are no more than 20 people at one session for the 4 simulation case blocks given the logistics of space.
Following the first session, other simulations can be scheduled as well as sessions with cases specifically tailored to unit needs or requests. Contact us for more information.